Which COVID-19 test should I take?
This holiday season has collided with a surge in COVID-19 cases. Many people have added another task to their travel and party planning to-do lists: Get tested.
As millions of people travel and join holiday and New Year celebrations, the contagious coronavirus may spread among loved ones gathering from near and far. And, the thinking goes, determining if anyone is bringing an unwanted guest (in this case, the virus) could help stop that chain of transmission. Receiving test results before events or travel can enable people to adapt their plans in order to prevent the virus from joining the festivities.
Neil Maniar (left), director of the Master of Public Health program and a professor of the practice in the Bouvé College of Health Sciences at Northeastern. Jared Auclair (right), associate dean of professional program and graduate affairs in the College of Science and an associate teaching professor of biotechnology at Northeastern. Photos by Matthew Modoono/Northeastern University and Adam Glanzman/Northeastern University
But negative COVID-19 tests don’t provide the final word. What a test does tell you can vary depending on what kind of test you use and when you take it—among other factors.
“It’s a snapshot in time,” says Jared Auclair, who runs Northeastern’s COVID-19 testing facility, the Life Sciences Testing Center in Burlington, Mass. And understanding how to interpret that snapshot can help you make decisions that keep your party and travel plans safer this holiday season.
How do the types of tests work?
There are two kinds of COVID-19 tests that are useful for detecting an active infection and preventing spread: PCR tests and antigen tests.
PCR tests (short for polymerase chain reaction tests) look for the genetic signature of the virus. These tests can detect the virus earliest after infection and PCR tests don’t require as much virus to be present in a patient. These tests can detect the virus about three to five days after someone is exposed, Auclair says, right around when someone starts to become infectious.
Typically, samples are collected and then sent to a laboratory where scientists conduct PCR tests. Results can take 24 to 72 hours to be returned to a patient. Northeastern uses PCR tests for its surveillance testing program.
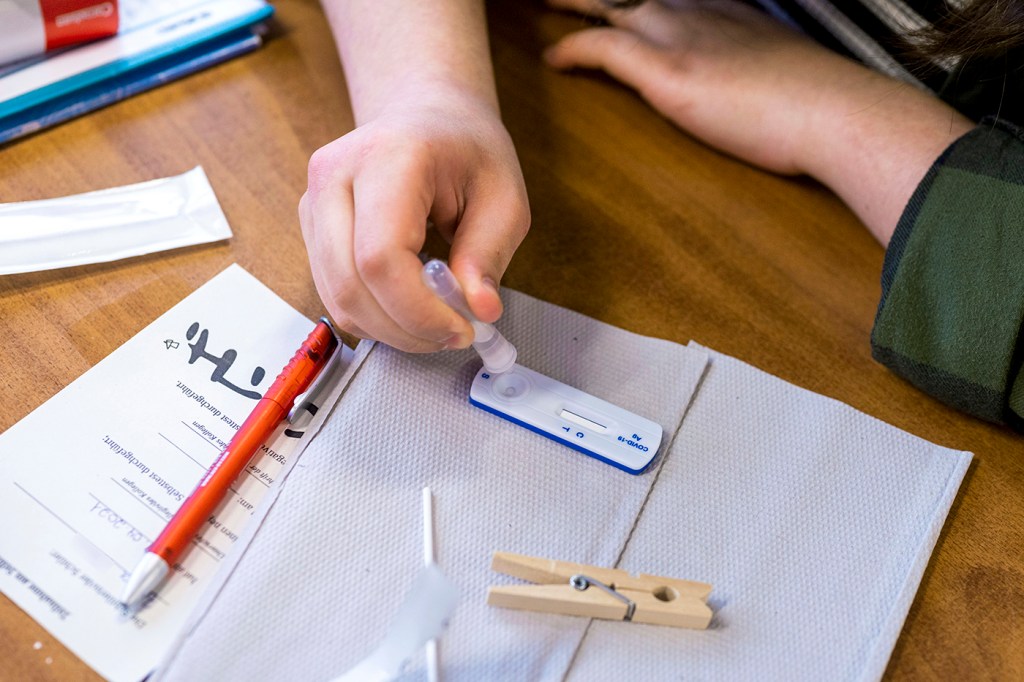
Antigen tests are what are typically referred to as “rapid tests.” Although rapid PCR tests do exist, they’re currently expensive and not readily available. Antigen tests can reveal a result in just 15 minutes, and many are sold at pharmacies for around $10 per test. Auclair says it takes about five to seven days after exposure to the virus for these tests to detect a COVID-19 infection.
While PCR tests look at the genetic material of a virus, antigen tests detect a specific protein on SARS-CoV-2, the virus that causes COVID-19.
“Because it’s looking for a protein, you sometimes need a larger sample,” says Neil Maniar, professor of public health practice, associate chair of the department of health sciences, and director of the master of public health program at Northeastern. “You can still do the nasal swab, but you need to make sure that you swab properly and for a proper length of time so that you are able to get enough of a sample.”
Is one kind of test better than the other?
Public health officials have called PCR tests the “gold standard” for spotting COVID-19 infections because they can detect a lower viral load in a patient. That means that they can spot the infection earlier and while someone is asymptomatic, as symptoms typically appear when the virus has had time to create a lot more of itself in the body.
Antigen tests are considered most reliable when used on a person who is symptomatic, because symptoms typically appear when someone has a higher viral load.
But that doesn’t necessarily make one test “better” than the other, Maniar says. “It really depends on the situation.”
I’m hosting a party where people will be eating, so they can’t keep masks on the whole time. Should I ask everyone to use a rapid antigen test at the door?
That would help reduce risk, Maniar says. But it wouldn’t eliminate it.
“You can get an antigen test the day of, and that will give you an indication that you don’t currently have an active infection,” he says. But “it may not capture an asymptomatic infection, so you may be infectious.”
For a party of vaccinated people who are not high-risk for severe cases of COVID-19, that might be just enough added security. Scientists think that people infected with COVID-19 are more contagious based on the higher viral load they have in their body. But there isn’t zero risk.
Asking guests to get a PCR test a day or two before the party could add more certainty that the ultimate unwanted guest is not in attendance, with the only wrinkle being the timeline. Since it takes some time to get results back for a PCR test, the “snapshot” that it represents will be farther from the actual time of the party.
I’m traveling to another household. How should I test before I go?
A PCR test as close to the trip as possible is best for this scenario, Maniar says, because it has a higher sensitivity and can catch an infection sooner.
If you don’t have access to a PCR test, however, Maniar suggests a series of antigen tests. Consider a sequence of three tests: You take the second test 48 hours after the first, and the third test 24 hours after the second.
“That will give you a much higher degree of confidence in the testing,” he says. “So if you have a negative result in all three of those, you can be much more confident that you do not have it.”
Does the omicron variant change the timeline at all?
It might.
“Omicron replicates much more rapidly than delta did,” Maniar says. “So with omicron, there’s a chance that you are going to be detectable much earlier than you would be with delta.”
Still, scientists have been studying omicron for just a few weeks so far. There’s still a lot to learn. So any change in timeline has yet to be pinned down.
For media inquiries, please contact Shannon Nargi at s.nargi@northeastern.edu or 617-373-5718.





