What makes cancer gene therapy so groundbreaking?
On July 12, a Food and Drug Administration panel unanimously recommended approval for the first-ever gene therapy treatment for cancer. The treatment, known as CTL019, is a T-cell therapy developed by the pharmaceutical company Novartis. It is tailored for each individual patient and has already been proven effective for treating a type of childhood leukemia. The New York Times reports that in a study of 63 patients, 52 of them went into remission after receiving the treatment.
Researchers have long been working to perfect gene therapy for a variety of cancers, but CTL019 will be the first to reach the market. If the FDA moves to approve CTL019, the decision could open the door for more gene therapy treatments for other diseases.
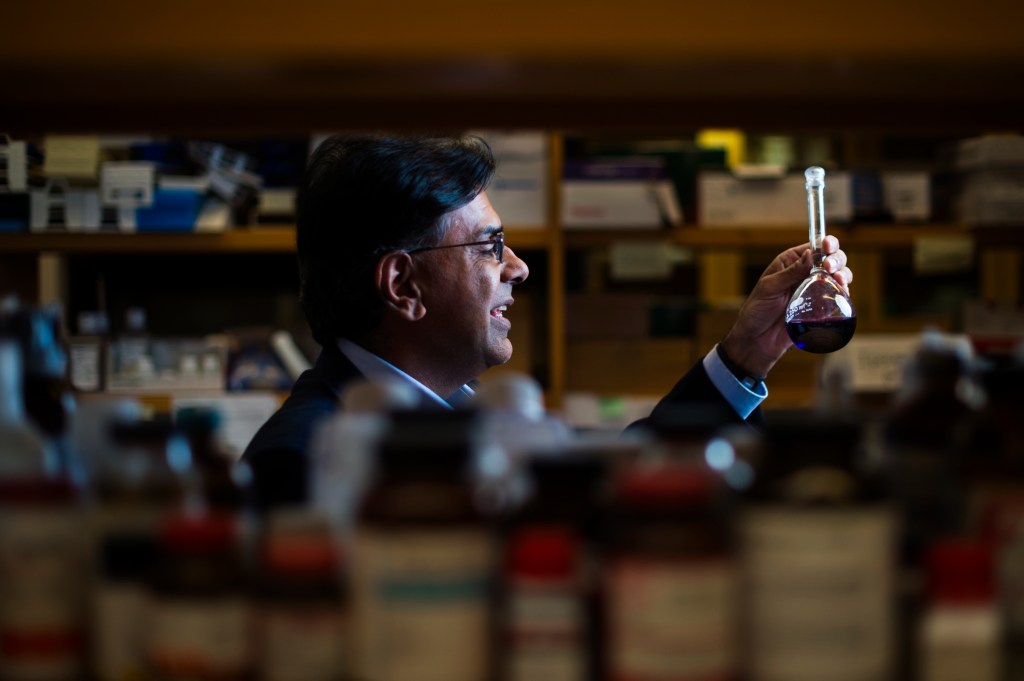
Mansoor Amiji is University Distinguished Professor in the Department of Pharmaceutical Sciences at Northeastern. His research focuses on the development of targeted therapies, including gene therapy, for treatment of the most lethal cancers, such as pancreatic, lung, ovarian, and brain tumors, as well as other chronic diseases. For one project, Amiji’s lab is interested in reprograming immune cells through genetic engineering to become more effective in treating cancer and inflammatory diseases.
Here, Amiji explains more about gene therapy treatment and why the approval of CTL019 would be so significant.
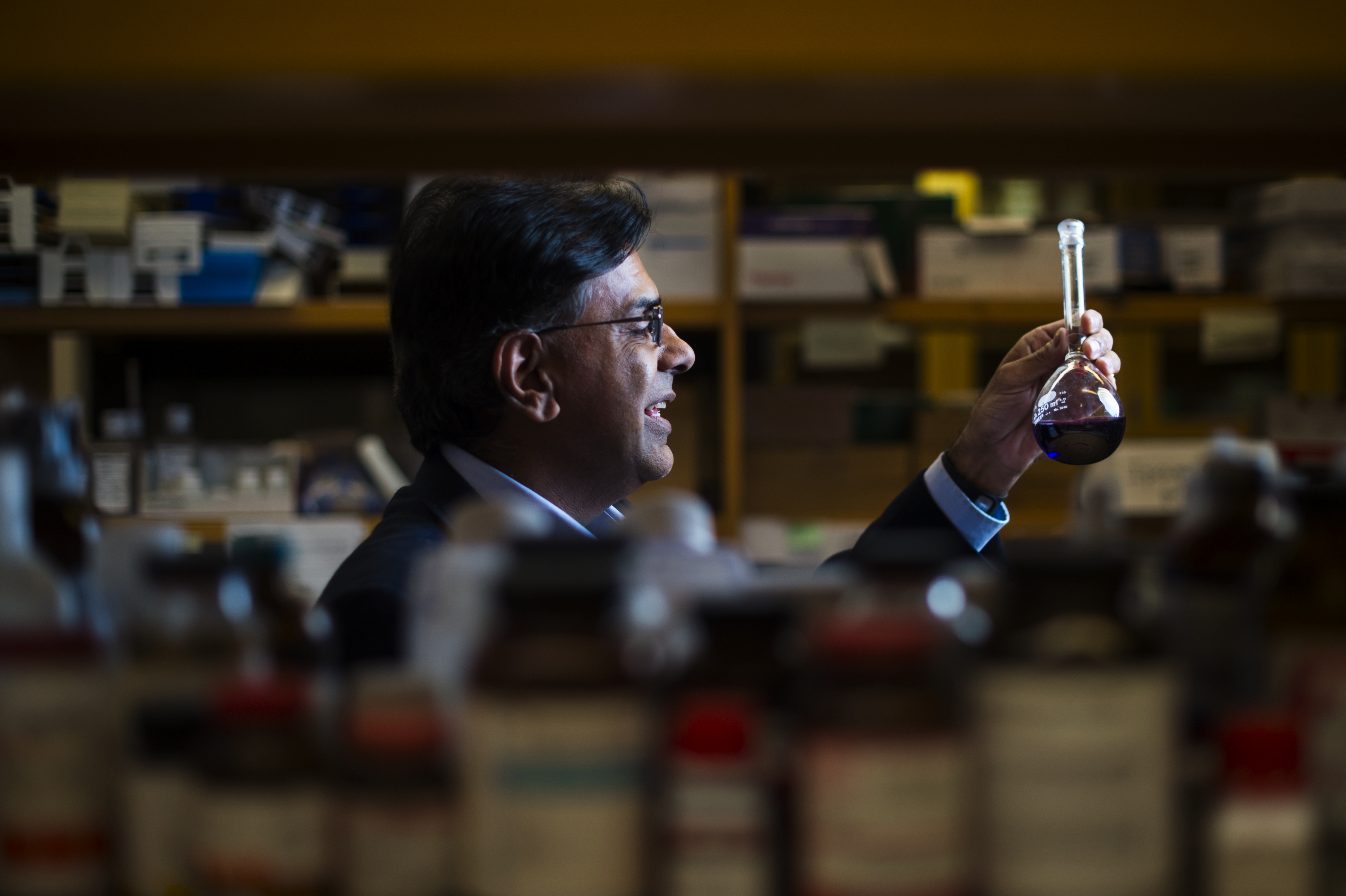
“It is still very early to suggest that cancer immunotherapy will lead to the ultimate cure or even long-term control of cancer,” says distinguished professor Mansoor Amiji. “But the opportunity to use the body’s own defenses to eradicate cancer cells is truly groundbreaking.” Photo by Adam Glanzman/Northeastern University
Can you briefly explain how CAR-T cell therapy works? It’s being called a “gene-altering” treatment. What does that mean?
CAR-T cell, or chimeric antigen receptor T-cell therapy, is one of the newer treatment options for cancer. It’s based on the patient’s own immune system. In this approach, the patient’s T-cells are harvested and then genetically modified outside the body to produce engineered cells. The cells are then re-administered and can destroy the tumor. There have been studies conducted at various medical centers over the past several years, but this is the first time that the FDA committee is allowing a commercial pharmaceutical company to continue with the program, in this case for treatment of pediatric acute lymphoblastic leukemia.
This therapy has already resulted in long remissions for many patients. Is gene therapy going to be the ultimate cure for cancer?
Yes, cancer immunotherapy treatments, including CAR-T cell therapy, have been very successful in cancer treatment. More than 85 percent of patients treated with genetically engineered CAR-T cells are under remission, and that is unprecedented for cancer treatment options. However, it is still very early to suggest that cancer immunotherapy will lead to the ultimate cure or even long-term control of cancer and change it from a “death sentence” to a treatable “chronic disease.” But the opportunity to use the body’s own defenses to eradicate cancer cells is truly groundbreaking.
Why is gene therapy so much more effective than other cancer treatments? What makes it different from the therapies we have been using for years?
Genetic engineering focuses on using modified cells as drugs. In this approach, the cells are either removed from the body and genetically manipulated outside, such as in CAR-T cell therapy, or genetic constructs are delivered into specific cells in the body. For the latter, the genetic construct has to be packaged in a delivery vehicle—nanoparticles, for example—and be targeted to the right cell in the body. Conventional drugs work by inhibiting a specific molecular target, like a receptor on a cell or an enzyme involved in disease progression. Genetic therapies like CAR-T cell therapy are focused more on the treatment at the DNA or RNA level where the original defects reside. That’s why they can be significantly more effective than conventional therapies, and they also promise to be a lot safer.
Why has it taken so long to develop and approve a gene therapy drug?
The drug development process starts from preclinical discovery and then moves into the clinical phase where patients are treated with experimental methods. Typically, it takes about 10 to 15 years for a drug to go from early discovery up to the approval stage. However, there are exceptions when compelling early-stage clinical results are obtained that encourage the FDA to approve the treatment a lot faster. Also, once a trail-blazing concept like CAR-T cell therapy is approved, there are many other companies that are following behind with their own version of the treatment. Their products will be coming to the marketplace soon as well.





