Local pharmacies and global systems: Two ways to improve COVID-19 vaccine distribution

As COVID-19 vaccines slowly make their way into the arms of people around the world, two faculty members at Northeastern consider ways to make distribution more equitable at the local and global levels.
Todd Brown, vice chair of the Department of Pharmacy and Health Systems, says that states should prioritize small, neighborhood pharmacies over large chains to distribute the vaccine while supplies are low and demand is high.
And Brook Baker, a law professor who studies intellectual property and access to medicine, argues for measures to encourage global cooperation so that wealthy countries don’t scoop up all the available vaccine doses and leave poorer countries behind.
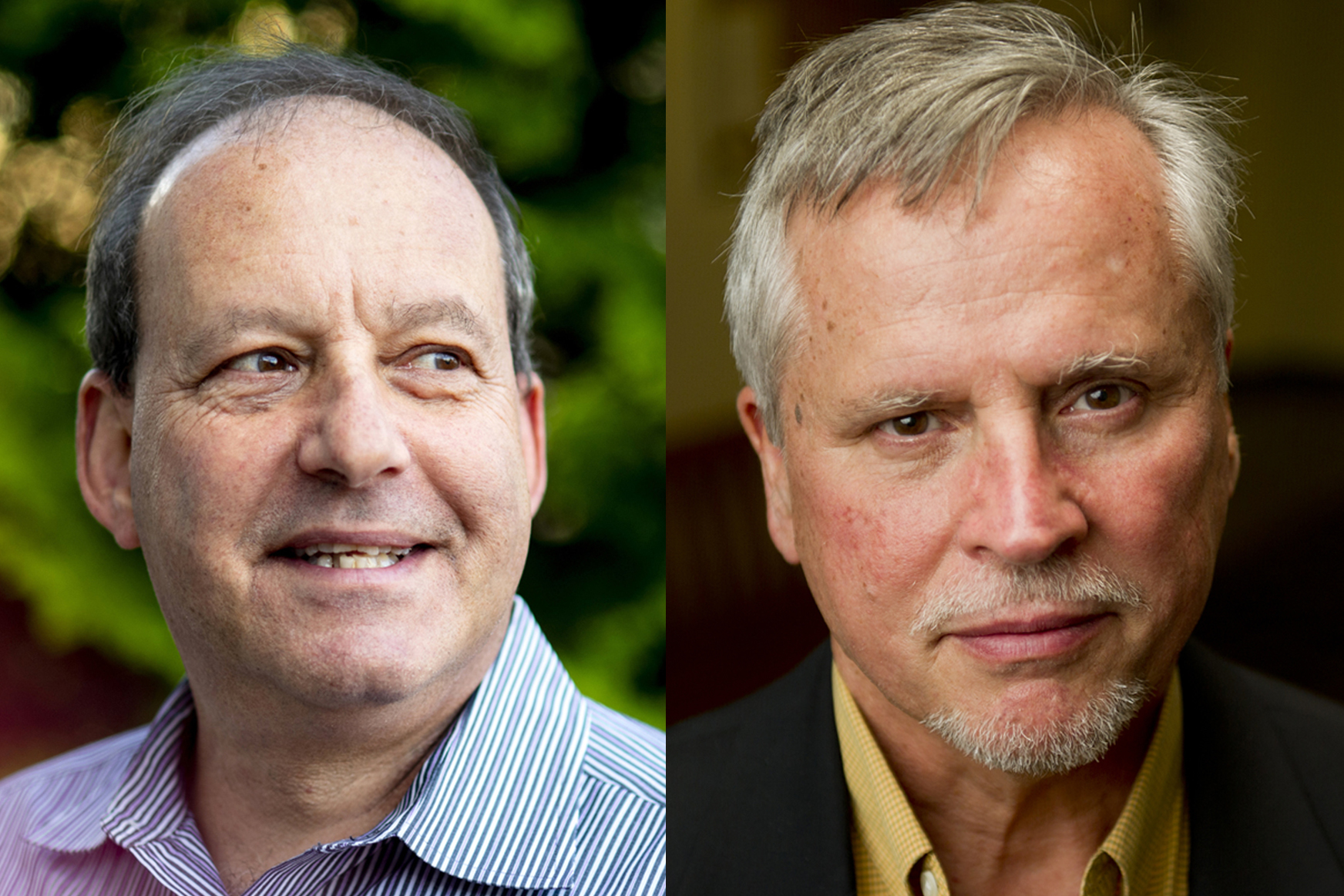
Left, Todd Brown, vice chair of the Department of Pharmacy and Health Systems Sciences. Photo by Ruby Wallau/Northeastern University Right, Brook Baker, a law professor who studies intellectual property and access to medicine. Photo by Northeastern
While they’re taking different angles on the solution, both Brown and Baker say that the problem of inequitable and inefficient vaccine distribution is one that affects everyone—the slower and more patchwork the immunization process, the more time the virus has to mutate and spread.
“There’s a crisis of inequality that plagues us in multiple areas,” Baker says, “but certainly in the context of a global pandemic like COVID-19, it’s one that leaves us all vulnerable to the disease.”
Distributing the vaccine has been a challenge on a global scale. Wealthy countries such as Canada and the U.S. have been able to secure hundreds of millions of doses of the vaccine (the Canadian government has secured enough vaccines to inoculate its entire population four times over), while more than 130 countries have yet to administer a single dose.
“This is a problem for all of us,” Baker says. “The more people who get infected, the more opportunity the virus has to mutate, and the more likely it is that the initial vaccines won’t work anymore.”
The World Health Organization has mobilized to create COVAX, an international effort to make vaccine distribution more equitable around the world. And Baker sees a few other possible solutions.
The Biden administration has already committed to helping fund COVAX. In addition, the U.S. could enact the Defense Production Act to expand manufacturing of the vaccines and procure the supplies necessary to produce them, Baker says. Three major vaccines—those created by Pfizer-BioNTech, Moderna, and Johnson & Johnson—were developed in the U.S. Ramping up their manufacture could mean more immunizations for people around the world.
The U.S. National Institutes of Health also could attach contractual requirements to its vaccine research funding that would oblige private companies to share their intellectual property with other drug companies, Baker says.
“There are, frankly, a lot of tools that a robust government response could produce that would help our domestic supply and the global supply over time,” he says.
For Brown, who also is the executive director of the Massachusetts Independent Pharmacists Association, the solution comes from communities. He says that states could have relied on their networks of independent pharmacies to distribute vaccines to their customers locally, both because smaller pharmacies are nimbler, and because the pharmacists who work at them better understand the populations they serve as compared to large chain companies.
Brown notes that some states did use the model. In West Virginia, public health officials relied upon independent pharmacies to distribute vaccinations throughout rural and elderly communities—to great success.
Independent pharmacists tend to have more personal relationships within their communities, Brown says, which can be critical when it comes to distributing the immunization to people who might otherwise be hesitant to receive it.
“A lot of times, people just want to talk to someone they trust, and in many communities, pharmacists are the people they can turn to,” he says.
Chain pharmacies do have their place in the rollout, Brown says.
“The strength of the big pharmacies is when it comes time to vaccinate the general population, and when our supply of vaccine meets the demand,” he says.
For media inquiries, please contact Jessica Hair at j.hair@northeastern.edu or 617-373-5718.





