This neuroscientist wants to change how we diagnose and treat mental illness

Imagine that a doctor could know which treatment would best help a patient with depression, anxiety, or some other mental illness by taking a picture of the person’s brain, not unlike the way people get an X-ray for a broken bone.
That, along with early detection and intervention tools, will be in the future of clinical psychiatric practice, said Susan Whitfield-Gabrieli, who started this semester as a psychology professor at Northeastern. And the work she and her colleagues will do together at Northeastern’s Center for Cognitive and Brain Health promises to play a role in helping prevent psychiatric disorders from progressing or developing at all.
Mental illness affects one in five adults in the United States and nearly 50 percent of all adolescents, according to the National Institute of Mental Health. Today, clinicians rely heavily on pencil-and-paper diagnostic tools, including questionnaires and other behavioral assessments, to pinpoint and treat psychiatric disorders. But success is often hard won, involving years of trial and error with medications and therapies before finding treatments that bring relief.
Whitfield-Gabrieli, a neuroscientist who is an expert in using brain imaging to understand how various regions of the brain are interconnected, hopes to change that. She said brain imaging science holds a key to bringing fundamental changes in how patients with mental illnesses are diagnosed and treated.
“Currently about half or more of patients are initially prescribed ineffective treatments,” Whitfield-Gabrieli said. “But cutting-edge neuroimaging methods may let us match patients with psychiatric diagnoses to individualized and optimally helpful treatments. Also, brain imaging may help identify children at risk for mental health problems, like clinical anxiety, so that preventive treatments can reduce the severity, or maybe even eliminate, such difficulties for those children.”
I’m hoping we can use brain imaging to inform what treatments psychiatrists use.
Susan Whitfield-Gabrieli, Neuroscientist
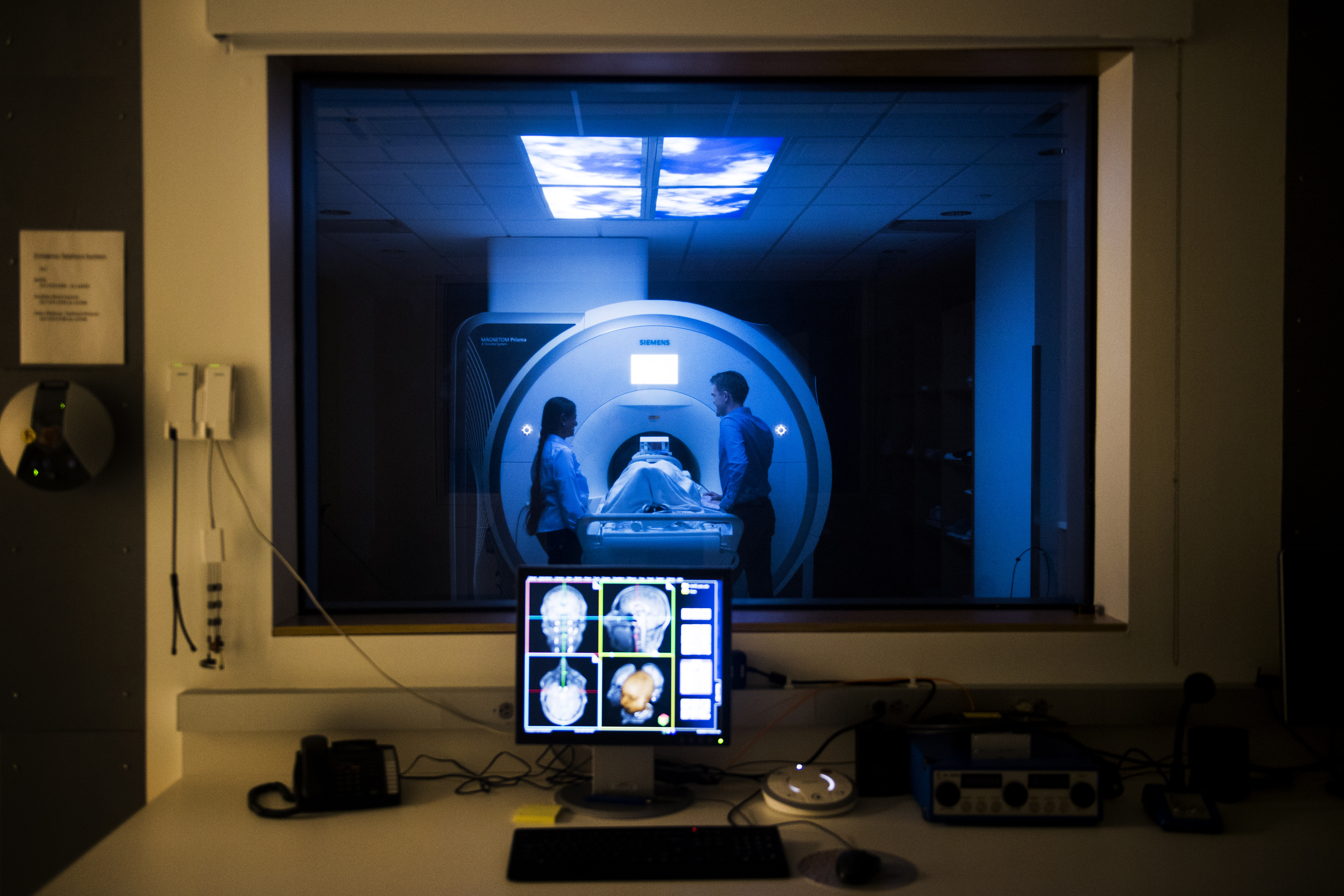
In her new role, Whitfield-Gabrieli will also lead the new biomedical imaging center housed within the Interdisciplinary Science and Engineering Complex. She wants to find ways to marry brain neuroscience research with real-world clinical applications, such as more precise treatments and interventions, as well as tools to predict and prevent mental illness. “That’s the bridge we need right now. We need to translate basic science into helping people live happier, healthier lives.”
The imaging center that Whitfield-Gabrieli is charged with directing is a first in human imaging for Northeastern and represents a significant investment, as costs to acquire and house the type of top-line equipment found at the center can soar to nearly $4 million. But Arthur Kramer, who directs the Center for Cognitive and Brain Health, said the facility is instrumental to the brand of research his team is doing to understand the effects of lifestyle, physical activity, and diet on the brain. The center’s new imaging tools will help researchers in their quest to understand how interventions—exercise, drinking water, and mindfulness techniques, for example—can lead to changes in the brain.
This is where Whitfield-Gabrieli’s experience in brain imaging science shines. She comes to Northeastern from the McGovern Institute for Brain Research at the Massachusetts Institute of Technology, where she studied what happens in the brain when it’s resting. When our minds wander or stop focusing on a task, a specific network of brain regions known as the default mode network becomes activated. But, in people with schizophrenia, bipolar depression, and other mental disorders, Whitfield-Gabrieli said this network becomes “hijacked,” causing auditory hallucinations, disturbed thoughts, and other troubling symptoms.
In an ongoing $6 million study funded by the National Institutes of Health, Whitfield-Gabrieli is examining how brain imaging and mindfulness techniques might help people with schizophrenia learn how to suppress auditory hallucinations. In this study, a brain imaging scan, known as functional magnetic resonance imaging, or fMRI, measures brain activity and provides immediate, real-time feedback to patients about what’s going on inside their brains. Using mindfulness techniques, patients can then train their brains to respond in a new way. Whitfield-Gabrieli hopes the work will lead to interventions that will allow the “hijacked” default mode network to function normally.
Backed by another $5 million grant from the agency, Whitfield-Gabrieli is leading a multi-institutional project that is looking for biomarkers in the brain—fingerprints, if you will—to predict anxiety and depression in adolescents and better understand who will respond to which treatments. The study is using data from the Human Connectome Project, a herculean effort to map the connections in the brain.
Chuck Hillman, the associate director of the cognitive and brain health center, described Whitfield-Gabrieli as “truly an expert in connectivity.” The positive effects of physical activity on brain health are well understood, he said, but Whitfield-Gabrieli lends “a new level of expertise” to the work being done at the center. “What’s going on in [the brain] is anyone’s guess,” he said. “She’ll help unravel it.”
Whitfield-Gabrieli focuses much of her research on children and adolescents with mental disorders. As a mother of two preteens, she sees this age group as particularly vulnerable to the deleterious effects of always-on technology and social media. “It’s quite dangerous,” she said, but she believes there’s a critical window of time when potential interventions—perhaps even the kind of interventions Hillman and Kramer are studying—can help reset a trajectory that would otherwise lead to mental illness.
“I think we can be trailblazers right here,” she said.
For Whitfield-Gabrieli, brain imaging just might be a family love affair: Her husband, John Gabrieli, is director of the McGovern Institute’s own imaging center, where Whitfield-Gabrieli remains a visiting scientist. She’s authored 134 papers, spoken at scores of conferences on brain connectivity and mental health, and even developed several open-source software tools that are widely used to process brain connectivity and imaging data.
Whitfield-Gabrieli envisions a future where “we have brain imaging as part of the psychiatric evaluation.” She believes researchers will be able to use the deepening pool of shared brain imaging data from efforts such as the Human Connectome Project to predict what’s going to happen in the brain’s neural pathways, which can then lead to the development of more effective and personalized treatments for mental illness. “I’m hoping we can use brain imaging to inform what treatments psychiatrists use.”





