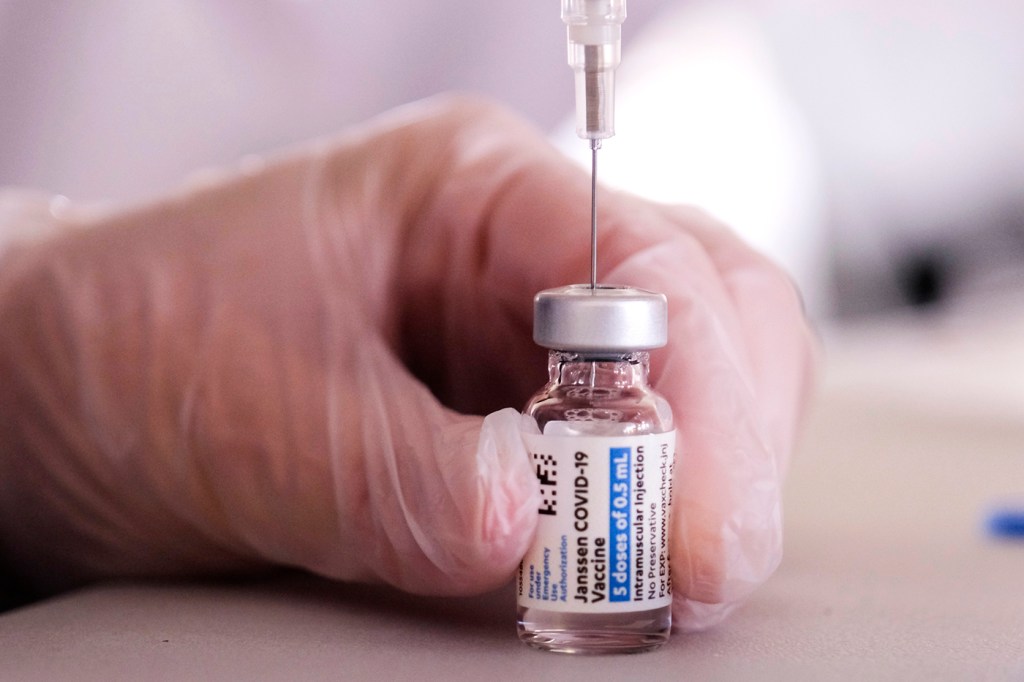
What does the Johnson & Johnson vaccine pause mean for all COVID-19 shots?
And then there were two.
Injections of Johnson & Johnson’s single-dose coronavirus vaccine stopped across much of the U.S. on Tuesday, after federal health officials called for a pause in the use of the vaccine, leaving the Pfizer-BioNTech and Moderna vaccines as the remaining inoculation options.
The announcement came as the U.S. Centers for Disease Control and Prevention, and the Food and Drug Administration said they are reviewing reports of six cases in which women who received that single-shot vaccine developed a rare, dangerous blood clotting disorder.
As April 19—the day that all adults in the U.S. will be eligible to receive a coronavirus vaccine—fast approaches, taking one of just three approved vaccines in the country off the table could complicate the public health campaign to vaccinate enough people against COVID-19 to reach a herd immunity threshold.
Taken at face value, there should be enough doses of the Pfizer-BioNTech and Moderna vaccines to go around. There is “more than enough supply to continue the current pace of vaccinations of 3 million shots per day,” according to a White House statement.
But it’s not that straightforward, says Nada Sanders, distinguished professor of supply chain management at Northeastern.

Left, Brandon Dionne is an assistant clinical professor of pharmacy and health systems sciences in the Bouvé College of Health Sciences at Northeastern. Right, Nada Sanders is distinguished professor of supply chain management in the D’Amore-McKim School of Business at Northeastern. Photo by Adam Glanzman/Northeastern University
Although the Johnson & Johnson vaccine makes up less than 5 percent of shots administered in the country so far, states’ plans for vaccinating the remaining public included the one-shot option. And public health officials may have to reassess how to allocate vaccine supplies to continue getting needles in arms as quickly possible. That third source of vaccines provided a buffer in the system.
“We’re putting really all our eggs in the basket of Pfizer and Moderna,” Sanders says. “We’re now dependent on Pfizer and Moderna, and that nothing goes wrong, in order to stay on track.”
And in supply chains, “something always goes wrong,” she says. The vaccine rollouts have already seen storms causing delays, a refrigerator being unplugged by accident, and manufacturing mistakes causing a massive batch of doses to be thrown out. So Sanders says more buffer will now need to be built into the manufacturing, logistics, delivery, distribution, and vaccine administering systems for both the Pfizer-BioNTech and Moderna vaccines.
More than 6.8 million people in the U.S. have received the Johnson & Johnson vaccine, according to the joint CDC and FDA statement.
All six cases of blood clots occurred six to 13 days after vaccination in women between the ages of 18 and 48. One woman died and another has been hospitalized in critical condition. This type of blood clot occurs in the brain and is called cerebral venous sinus thrombosis (CVST). It was observed in combination with low levels of blood platelets in the patients. CVST is a rare form of stroke and can cause permanent damage to the brain and central nervous system. It can be treated, but requires a different approach to other blood clots.
“It is very serious, so I think it’s the right step to look into this more,” says Brandon Dionne, assistant clinical professor of pharmacy and health systems sciences at Northeastern. “But I don’t want to scare people into thinking, ‘Oh, this is going to happen to you.’ It’s still an incredibly rare event.”
Six cases out of about 6.8 million doses administered means that, if researchers decisively connect the blood clots to the vaccinations, the risk is less than one in a million (it actually works out to 1 in 1.1 million). And with something that rare, it’s not surprising that the risk would only surface once the vaccine is rolled out to millions of people, Dionne says. About 45,000 people were enrolled in the Johnson & Johnson vaccine trial.
“It’s not uncommon to see adverse effects that weren’t seen in the clinical trials when you roll it out to a larger population, especially something as rare as this,” Dionne says. “There’s not really much that could’ve been done differently in the clinical trials to have prevented this from happening.”
The move to halt distribution of the Johnson & Johnson vaccine could further fuel vaccine hesitancy, Dionne worries. But, he says, responding to a frequent concern about the coronavirus vaccines, “This was not because the process was rushed.”
Even running the trial for a few years and garnering regular FDA approval rather than Emergency Use Authorization wouldn’t have changed anything, he says. In the six women who experienced CVST, the symptoms appeared in less than two weeks after vaccination.
These new questions about the Johnson & Johnson vaccine echo concerns about blood clots associated with the vaccine developed by AstraZeneca and Oxford University. The European Medicines Agency confirmed last week that the brain blood clots are a rare side effect of that shot.
“It’s not really clear exactly what’s causing it,” Dionne says. But there are similarities between the AstraZeneca-Oxford vaccine and the Johnson & Johnson vaccine that could hold clues. Both vaccines use an adenovirus delivery method. The Pfizer-BioNTech and Moderna vaccines, on the other hand, are mRNA vaccines that use a lipid particle delivery approach. So, he says, it’s possible that that distinction could explain why the blood clots have been associated with both the AstraZeneca-Oxford vaccine and the Johnson & Johnson vaccine but not the Pfizer-BioNTech and Moderna vaccines.
More than 99 million Pfizer-BioNTech vaccine doses and more than 85 million Moderna doses have been administered in the U.S., compared to Johnson & Johnson’s approximately 7 million, according to the CDC. No cases of the brain blood clots have been reported with those two-shot vaccines.
Johnson & Johnson’s vaccine will likely be back in play at some point after review of these cases. The U.S. may choose to follow the approach some other countries have taken regarding the AstraZeneca-Oxford vaccine and restrict the Johnson & Johnson vaccine to older patients who are at a higher risk of having a severe case of COVID-19 and a lower risk of blood clots, suggests Dionne. Or perhaps it could be opened up to male patients and post-menopausal female patients, as all six cases were primarily in pre-menopausal women and estrogen has previously been associated with risks of blood clots, particularly associated with hormonal contraceptives.
“I think there still is a role for J&J, and I think there is also a piece of informed consent and decision-making here,” Dionne says. For someone who is at lower risk for a blood clot and may prefer that vaccine, they may be able to make their own decision.
The one-shot Johnson & Johnson vaccine has also been an option for people who were wary about the two shot options, particularly because that single-dose option boasted fewer side effects. This pause in distribution of that vaccine might increase such wariness. “The biggest fear for me is that this is going to increase vaccine hesitancy,” Dionne says.
“But I’m hopeful that people will also take heart in the fact that the FDA paused as soon as they were made aware of this,” he says. “It goes to show that they are monitoring and they’re not trying to force this through and get everyone vaccinated, damn the consequences.”
For media inquiries, please contact media@northeastern.edu.





