A breakthrough in bioprinting may soon lead to 3D-printed blood vessels and human organs
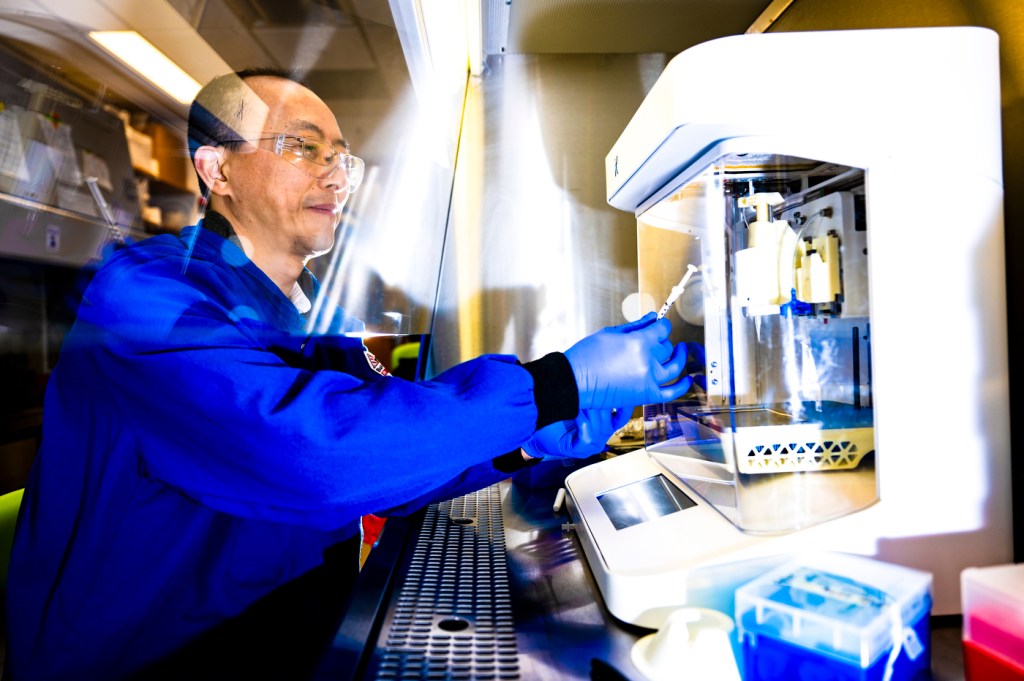
Northeastern professor Guohao Dai has helped lead the development of a new elastic material designed for 3D printing of soft living tissues.
A breakthrough in bioprinting of living tissues could soon lead to 3D-printing of blood vessels and human organs, ushering in a new era of regenerative medicine.
Guohao Dai, a bioengineering professor at Northeastern University, and his collaborators recently patented a new elastic hydrogel material designed for 3D printing of soft living tissues.
Modern medicine uses three-dimensional printing to create hard implants such as cranial plates and hip joints, limb prostheses and medical devices.
However, 3D printing of organs and soft tissues is still a major challenge, says Dai, whose research focuses on 3D bioprinting, stem cells and vascular bioengineering.
Current 3D printers use polymers, plastic filaments, powders or resin to build printed objects that harden as they cool. Soft tissues, Dai says, require elastic materials that can stretch and recoil — something existing materials lack.
“Elasticity is very important for maintaining the normal function of the tissue,” Dai says.
Solving this challenge can revolutionize medicine and make organ transplants obsolete.


Hydrogels are synthetic polymers capable of holding water, Dai says. They are used, for example, for facial masks that contain skin nutrients, wound dressings that deliver drugs, and soft contact lenses that contain significant amounts of water for comfort and oxygen transmission.
But traditional hydrogels, Dai says, are too fragile for 3D printing. They can’t withstand stretching or twisting, limiting their medical applications.
To solve this issue, Dai joined forces with Yi Hong from the University of Texas Arlington. While Hong found a way to make soft hydrogels elastic, Dai used his expertise in 3D printing to further modify certain properties of these hydrogels so they could go through a printer.
To go through the printing nozzle, Dai says, the material had to be liquid but it also had to keep its shape after an object was printed.
The new material dissolves in a liquid solution and can encapsulate a large amount of water after printing. This is good for growing cells, Dai says, because it mimics the environment of the human body that on average consists of 60% of water.
Cells get infused into the liquid solution before printing. Once printed, the object is exposed to blue light, triggering a photochemical reaction that makes the gel elastic without harming the living cells.
“You can print any geometry,” Dai says.”You can print a tube or a blood vessel.”
The cells then multiply and grow inside the printed structure.
“We grow them under the pulsatile pressure to mimic the human’s blood pressure,” Dai says.
Another key advantage of the new elastic hydrogel is that it’s biodegradable. Since it’s a foreign polymer, Dai says, the goal was to make it completely degradable while cells replace it with their own collagen and elastin, forming a strong, natural blood vessel.
“It’s not native to your body, that is why we wanted it to eventually be gone completely,” Dai says.
So far, the printed blood vessels cultured for two weeks remain relatively weak, Dai says, and can’t yet withstand human blood pressure. He believes that extending the culturing period to two months, which is an expensive experiment, could allow the cells to fully develop a strong structure.
Additionally, researchers are working to speed up hydrogel’s degradation, aiming for it to dissolve within two to three months while the cells mature into functional blood vessels.
Dai says this technology will eventually enable the creation of blood vessels for patients using their own cells. As the hydrogel degrades, the body will naturally replace it, resulting in fully functional tissue or organs.






