From EKG tabs to silent seizure detectors, Northeastern students offer solutions to improve health care in rural Maine
A group of bioengineering students have developed Silicon EKG tabs to replace EKG stickers after visiting rural healthcare centers in Maine.
An electrocardiogram is a non-invasive test that helps doctors detect problems with a person’s heart rate or rhythm. But there is some prep work involved that some patients find uncomfortable and makes the process longer.
EKG stickers need to be placed on a person’s chest, arms and legs, and for accurate readings, body hair in those areas often needs to be removed.
That can be difficult in rushed situations, like when EMTs are performing lifesaving care in the back of an ambulance, or in fast-moving environments like a hospital emergency room, explains Northeastern University graduate Jason Xu.
Sometimes the stickers fall off because of sweat or movement and need to be reapplied, wasting critical moments the patient may not have.
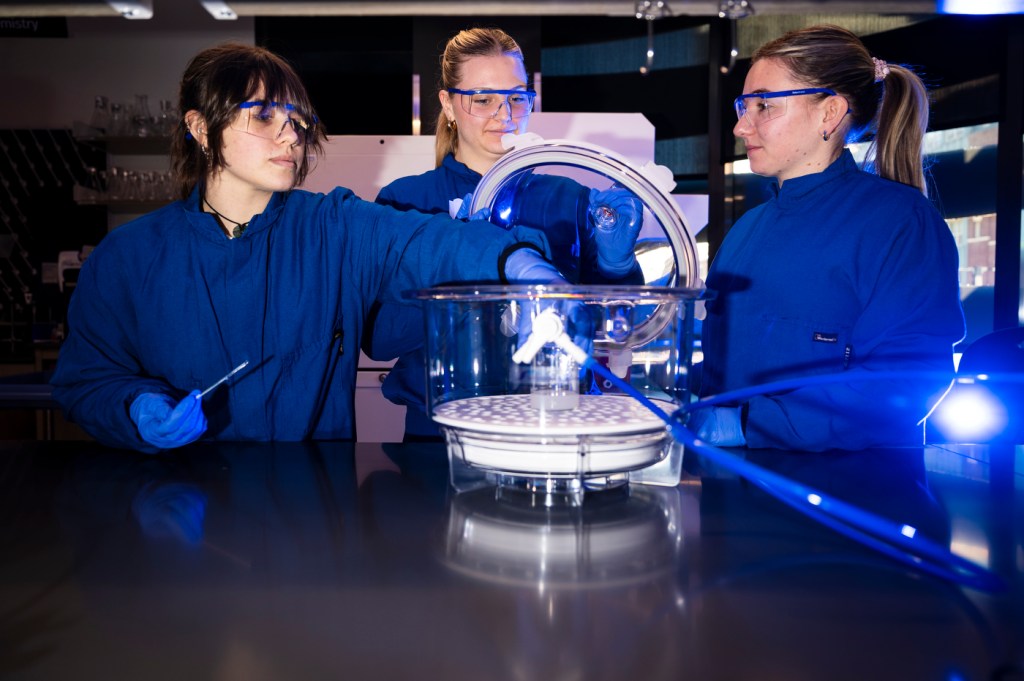
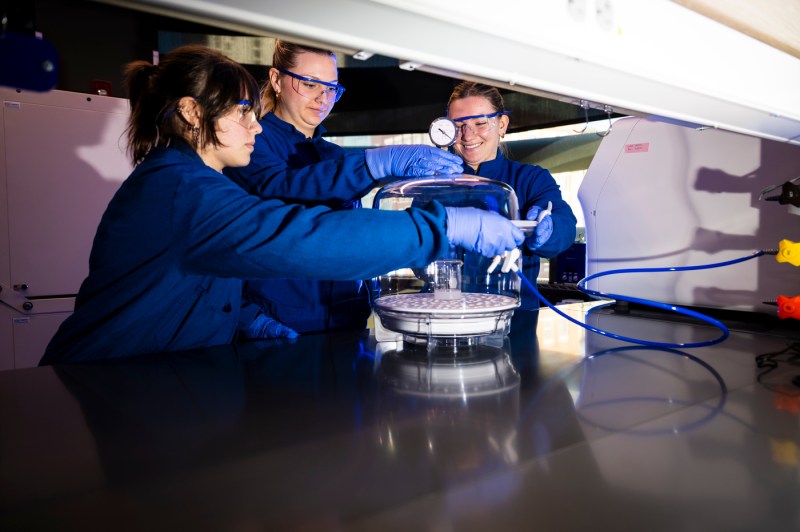
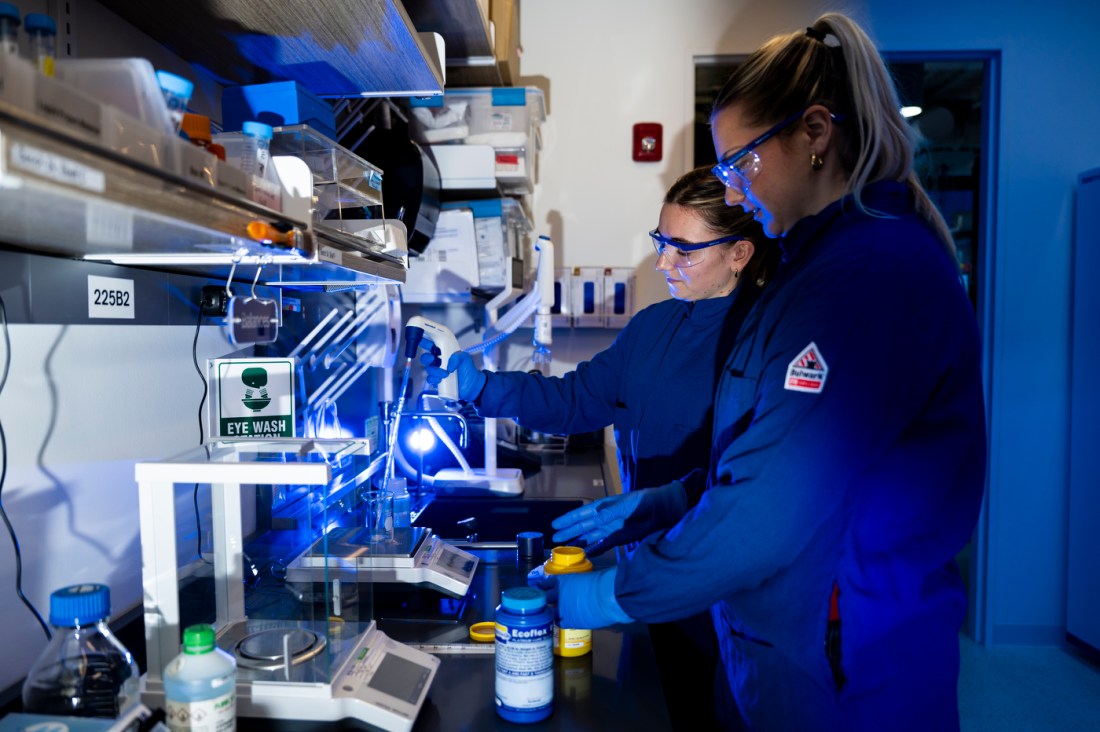
For his senior capstone, Xu and a group of bioengineering students at Northeastern developed a solution — the Flextab, a circular silicon-based EKG tab that medical professionals can use in place of stickers.
The tabs aren’t sticky and aren’t affected by body hair, improving both the patient experience and helping medical professionals work more efficiently, the students say.
That was one of several innovative ideas the group of five students thought up after shadowing medical professionals in rural Maine last year as part of a capstone course at Northeastern’s Roux Institute.
The trip, which included visits to MaineHealth Pen Bay Medical Center, Oasis Free Clinic and LifeFlight, served as an opportunity for students to see firsthand the state’s health apparatus and develop potential solutions to some of its biggest problems.

Much of Maine’s population — like many rural states — is economically disadvantaged and many people live miles away from any health facilities, explains Katherine Simmonds, the associate director of health services at the Roux and a clinical professor in Northeastern’s Bouvé College of Health Sciences.
The hospitals that are nearby are under a lot of financial strain, and are reducing their offering of more specialized services. Broadband access is also spotty in many parts of the state, making options like telehealth limited. Many residents also rely on Medicare or Medicaid, which don’t provide the best coverage.
“Those factors — what we call social determinants or social drivers of health — really feed into people’s ability to access health care,” Simmonds says.
One way to address these disparities is collaborating with engineers, computer scientists and public health experts, she says. That sentiment is at the heart of the students’ capstone trip, which was supported by a National Institute for Health grant.
“Maine has the oldest mean age demographic in the nation, meaning that we are not only rural, we’re old rural,” Simmonds says. “We are not replacing people who fill out the workforce, which means we really need talent, innovation and people who think differently.”

Before students shadowed the medical facilities, they took Introduction to Rural Health, a course taught by Simmonds where they learned “about the challenges in addressing rural health disparities, and how to approach solutions from an asset-based framework.”
“We start with just understanding what do we mean by rural? We think about the concepts of rurality and how rurality is measured and really examine it. Then we delve into health inequities and rural health inequities and start talking about problems and solutions,” she says.
Students kept those lessons in mind as they visited the facilities. At Pen Bay Medical Center, students went to the hospital’s emergency room and intensive care unit, meeting with health caregivers and patients.
That’s where the idea for the EKG tabs was born, explains Lauren Piasecki, a fourth-year bioengineering student.
“A lot of people were complaining about EKG stickers,” she says. “When we were talking with the technicians, there were a lot of struggles of putting them on, having them stick and replacing them,” she says.
Editor’s Picks
While the five students decided to focus on the EKG project for their capstone project, they developed three other capstone project ideas that other students decided to pick up.
Two of those projects were born out of an interaction the students saw between a patient and a nurse. The patient was unresponsive, and the nurse was struggling to understand whether she didn’t want to speak or if she was having a silent seizure.
“This evolved into us thinking, ‘Oh, is there a way we could maybe detect silent seizures to make it easier for nurses to understand if it’s more of a patient’s choice not to respond or is something medical going on?’”
From that question, one capstone team decided to develop a silent seizure detection device, and another developed a silent seizure simulator to model epileptic brain wave activity.
In the hosptial’s diabetes center, the students heard from patients about their transportation challenges. Many had traveled long distances to have a blood sugar monitoring device installed, which is very difficult to apply on your own, explains Megan Burke, a fourth-year bioengineering student.
From that pain point, the team proposed the creation of an additional device that could help patients place those blood sugar monitoring devices on their own, which another capstone team picked up.
For the group, it was a worthwhile experience and let them see the real-world impact their research could have.
“We went somewhere, saw an unmet clinical need, and transformed that into an idea, and then transformed that into a functioning prototype, and we learned a lot of skills along the way,” says Burke.