How will AI transform health care? Northeastern to host workshop and conference focused on precision health
Ideally, artificial intelligence should make going to the doctor an easier and less stressful experience.
“If AI is working the way that we envision it, you actually won’t notice a lot of direct impact,” says Sam Scarpino, the AI+Life Sciences director at Northeastern University’s Institute for Experiential AI. “What you’ll notice is that more pharmaceuticals are coming to market for treating increasingly rare diseases. You’ll notice more time with your physician. We will be catching cancer earlier, when it’s more treatable.”
In a best-case scenario, AI should run in the background “the same way that a good car runs smoothly without you thinking about what’s under the hood or what is keeping the wheels moving,” adds Gene Tunik, the AI+Health director at the institute.
Yet the reality is that for as much progress we have made in AI — with its uses to develop drugs, help diagnose cancers and optimize medical data management — it is not used in every hospital or embraced at every clinic.
There are still many challenges to overcome in terms of the accuracy and reliability of AI-based technologies, the costs of deploying them on a large scale, and the constraints in harnessing high-quality data for their development.
Editor’s Picks
So, what needs to be done to help us get there?
Next month, the Institute for Experiential AI will invite a host of health care and AI experts to Northeastern’s Boston campus to discuss just that at The Future of AI in Health & Life Sciences Workshop and The State of AI in Precision Health Conference.
Tunik notes that “we are in a watershed time” for AI and its impact on the health care industry.
“A lot of health care organizations are now starting to create roadmaps for themselves in terms of their AI and health strategy and how to implement them,” says Tunik. “A lot of these are being done in partnership with some of the big companies. Academia is also a big part of these conversations because it holds a lot of think tanks for this area, so the timing of this conference is really opportune.”
“It’s not so early that it’s all conceptual,” he adds. “There is already some rubber hitting the road here, but it’s not so far along that the ship has sailed.”
The activities kick off with the workshop on Oct. 9 at the EXP building, where attendees will discuss the best approaches to integrating AI into health care training, explains Scarpino.
“Much of the existing workforce will need to upskill around AI literacy,” he says. “Individuals coming through their undergraduate and graduate education, regardless of major, are going to need to have AI literacy. How do we embed that into all our curriculum in a way to ensure students are still getting the critical and analytical thinking skills they need to have to function in our modern society?”
The conference will be held the following day, Oct. 10, on the 17th floor of East Village, and focus specifically on precision health, an umbrella term meant to describe a form of medicine that is highly individualized and targeted.
The all-day event will feature health care and life science executives from the Mayo Clinic, Brigham and Women’s Hospital, Advocate Health and more. Topics that will be discussed include AI’s use in drug discovery and development, how AI can be used for aging in place and medicine in place, and AI’s ability to be used in patient care — from diagnosing conditions and developing treatment plans to predicting outcomes and triaging tasks.
Raimond Winslow, director of life sciences and medicine research at Northeastern’s Roux Institute and a core faculty member at the institute, adds that medicine and health care are increasingly becoming “computational disciplines.”
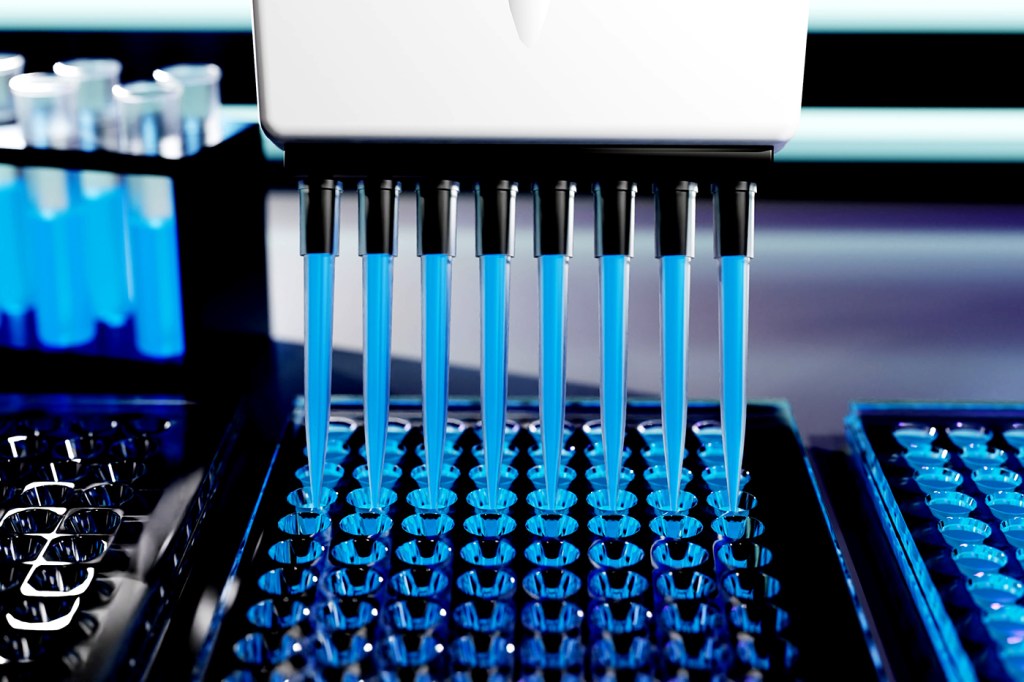
“This is going to happen,” he says. “It’s a transformation that will happen, and is underway. It happened in biology 15 to 20 years ago. Biology started making the transition from being purely an empirical and wet lab science-based to becoming to a great extent also a computational science.”
“This is happening in medicine, and what this means is that caregivers of all kinds are always going to be at the tip of the spear delivering health care but increasingly their decisions are going to be informed by AI methods, algorithms running on data from that patient.”
Precision health is a particularly strong application area for AI since it requires physicians to analyze large amounts of patients’ data quickly and hit very targeted, specific, and unique health objectives, explains Usama Fayyad, the institute’s executive director.
“That’s an area where being able to process a lot of data on a per patient basis is something that is not pragmatic for a normal healthcare provider, but if AI was there, it could help suggest directions and answers,” he says. “That could be a beautiful place to use it.”