Experimental antibiotic treatment for Lyme heads for human safety trials

Human safety trials of a novel antibiotic treatment for Lyme disease developed by Northeastern professor Kim Lewis are scheduled to start this spring in Australia, with results anticipated by fall.
“Hopefully, the results will be positive,” says Lewis, University Distinguished Professor of Biology.
So far the therapeutic agent, an antibiotic known as hygromycin A, has not been toxic in animals and has cleared Lyme in mice, he says.
Existing standard treatments for Lyme disease, doxycycline and amoxicillin, have proved far from silver bullets for the nearly half-million people stricken by the tick-borne illness in the U.S. each year.
The Centers for Disease Control and Prevention estimates that 5% to 10% of Lyme patients have persistent symptoms after early treatment, while the Global Lyme Alliance says that as many as 2 million Americans could suffer post-treatment disability.
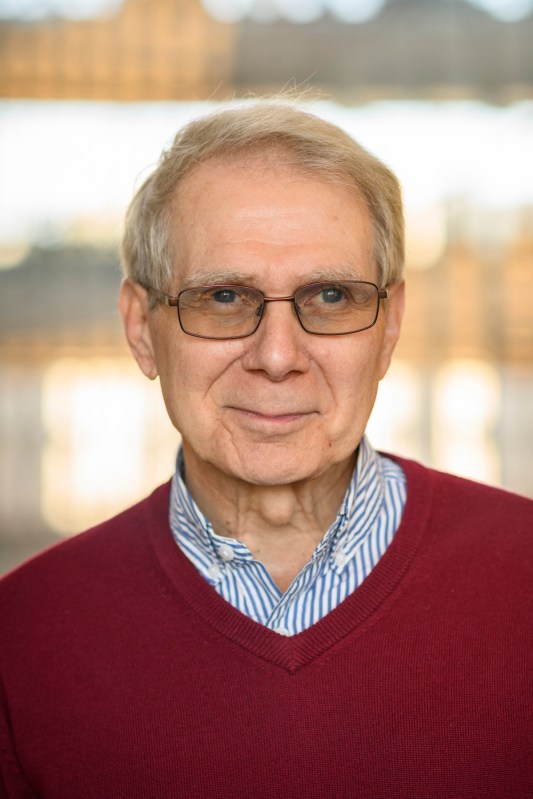
Lewis says that hygromycin A is different from the broad spectrum antibiotics in that it specifically targets spirochetes including Borrelia burgdorferi, the spiral-shaped bacterium that transmits Lyme disease through the bite of a deer tick.
The expectation is not only that hygromycin A will prove more effective in curing Lyme disease in the early, acute stage but that it could also mop up residual pathogens that may persist in some patients with chronic disease, Lewis says.
He suspects many cases of chronic Lyme symptoms are caused by changes to patients’ microbiomes due to the use of broad spectrum antibiotics.
Featured Posts
With hygromycin’s specific targeting of spirochetes, Lewis says that is less likely to lead to chronic disease.
“What we’re testing for now is a treatment for acute Lyme that will be more effective and won’t wreck the microbiome and will hopefully lead to fewer chronic cases,” he says.
People with chronic, long-term or persistent Lyme call it a life-changing experience, leaving them with arthritis, cardiac problems, fatigue, brain fog, depression and anxiety.
Made by a bacterium found in the soil, hygromycin A has been a known but overlooked antimicrobial since 1953, Lewis says.
“Nobody really cared about this compound because it’s very weak against regular bacteria. What we discovered is that it is indeed very weak against regular pathogens but exceptionally potent against spirochetes.”
Lewis’ team has licensed the compound to Flightpath, a biotech company focused on Lyme disease that is conducting the phase 1 trial scheduled to start in April. Flightpath is leading the clinical development effort with funding from the Cohen Foundation.
“A safety trial simply asks the question, ‘Is it safe for healthy people to take this drug,’” Lewis says.
If it passes toxicity screenings, it can advance to phase 2 to determine effective dosing ranges “and see if it cures acute Lyme disease,” he says.
Success at that stage would lead to a clinical trial involving a larger group of patients, with the possible end result of requesting FDA approval for the treatment via a new drug application.
Even if approved, human efficacy trials probably wouldn’t start until 2025, Lewis says.
That hasn’t stopped the Global Lyme Alliance, which helped fund Lewis’ Lyme drug discovery program, from expressing excitement over the prospect of seeing hygromycin A in doctors’ hands.
In a statement on Instagram in February, the alliance quoted Flightpath CEO Matt Tindall saying that reaching this stage is a “landmark achievement for Lyme patients.”
If the trials make it to phase 2, researchers will reach out to Lyme specialists at places such as Johns Hopkins and Massachusetts General Hospital to recruit Lyme patients for the study, Lewis says.
Most projects that researchers in academia and industry toil on for years “do not get to the point when we feel, based on extensive animal studies, that the compound has sufficient efficacy and safety features that we can now introduce it into humans,” Lewis says.
“We are at that point with hygromycin A. That is, of course, encouraging,” he says.