Nanomedicine could reduce the frequency of breast and ovarian cancer treatments, research finds
A Northeastern University researcher is using nanomedicine to develop a time-released immunomodulatory treatment that would lengthen time between hospital visits for patients fighting advanced breast cancer.
Most cancer drugs require continual daily or weekly delivery, leading to frequent hospital visits, says Needa Brown, an assistant teaching professor of physics at Northeastern.
“It’s not the best quality of life for the patient,” says Brown, who is also Northeastern’s program director of the Nanomedicine Graduate Certificate and Master of Science program, which launched in the fall.
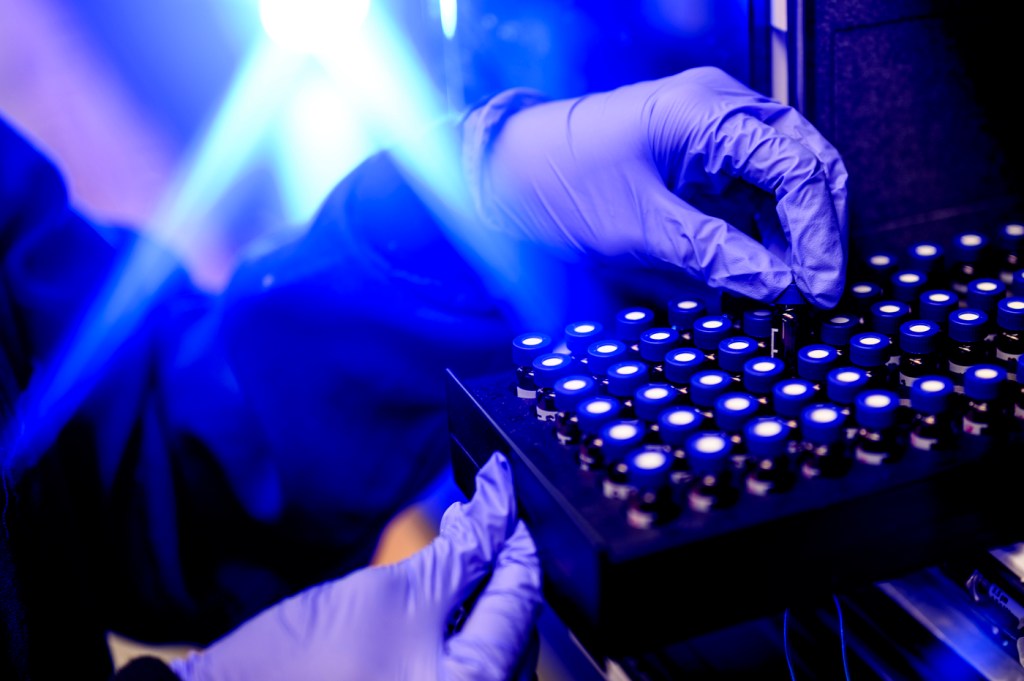
Her lab is working on using nanomedicine to deliver an immune-revving drug, called a STING agonist, via a time-release formulation that could potentially reduce patient visits to once a month.

“It reduces patient burden, so they don’t have to come in over and over to get these treatments,” Brown says.
The other drug taken by advanced breast cancer patients, a chemotherapy agent known as a PARP inhibitor, can be taken orally at home, she says. “So there’s no reason for them to come to the clinic as frequently.”
The research on developing a biomaterial formulation to deliver the STING agonist is being funded by a three-year Department of Defense breakthrough grant, Brown says.
Northeastern is partnering on the research with Dr. Jennifer Guerriero — a Northeastern graduate — at Brigham and Women’s Hospital in Boston and Northeastern Distinguished Professor Srinivas Sridhar.
The ultimate goal is to use the nanomedicine approach in clinical trials, says Brown. She says the $2.5 million grant will be split between Northeastern and the hospital.
Brown calls the partnership an exciting example of the potential for nanotechnology, which enables the manipulation of atoms and molecules at nanoscale, or 100 millionth of a millimeter, to benefit patients in a medical setting.



“Nanoparticles are great vehicles to deliver drugs in ways that reduce toxicity and enhance efficacy and delivery to the right target,” she says.
Her lab also has a second recently awarded Department of Defense grant totaling $389,825 to fund two years of research on a pilot project using lipid particles to deliver drug treatment for metastatic ovarian cancer.
Nanomedicine at Northeastern
Brown says Northeastern has been a pioneer in nanomedicine education since 2005 with over $9.8 million in education grants due to programming developed by Sridhar, a distinguished professor of physics, bioengineering and chemical engineering, and director of the Nanomedicine Innovation Center, and Anne L. van de Ven, an associate teaching professor of physics and co-director of the Nanomedicine Programs.
Editor’s Picks
As of the fall 2023 semester, in addition to the Nanomedicine Graduate Certificate, Northeastern now also offers a regular master’s degree in nanomedicine and has brought on a new faculty member, Kinan Alhallak, assistant teaching professor and nanomedicine researcher, to accommodate the demand, Brown says.
“There are five universities that offer graduate curriculum in nanomedicine in the U.S., with Northeastern being the only one offering a formal graduate certificate and masters program,” she says.
The master’s degree includes a co-op requirement that distinguishes it from programs being offered by other universities, Brown says.
She says popular interest in nanomedicine has grown with the development of mRNA vaccines for COVID-19 that use nanotechnology to improve the vaccine’s stability and facilitate delivery of mRNA to the target site.
The Nobel Prize in Physiology or Medicine was given for the development of the mRNA vaccines and the Nobel Prize in Chemistry was awarded this fall for quantum dots, which are also nanoparticles, Brown says.
She says using nanomedicine to develop a time-release delivery of STING agonist agents to breast and ovarian cancer patients involves two approaches, a lipid formulation for a systemic solution and biodegradable implants for sustained local treatment.
“It’s essentially taking a very different route to immunotherapy,” which has had a lot of hype but less application because of various toxicities associated with it, including in combination with other drugs, Brown says.
“The STING agonist (short for Stimulator of interferon genes pathway) has shown promise, however it so far hasn’t translated” into effective treatments, she says.
“The reason for that is that it’s really difficult to overcome the delivery barrier,” Brown says.
“Systemic delivery of the STING agonist triggers widespread immune responses which makes the drug intolerable. On the other hand, direct tumor injections require a patient to come into the clinic very frequently to receive treatment. The nanomedicine approach aims to circumvent systemic toxicity and reduce patient burden, allowing for the successful clinical translation of STING agonists,” she says.
Brown says the goal of the research is to see if “nanomedicine is the bridge that’s necessary to get this really promising drug into the clinic.”