Why do some vaccines (polio, measles) prevent diseases, while others (COVID-19, flu) only reduce their severity?

When the first vaccines for COVID-19 rolled out in December 2020, some people hoped they would be a silver bullet against the novel virus the way that polio and smallpox shots are nearly 100% effective against those diseases.
Instead, the updated COVID vaccine is being compared to the flu vaccine in the sense that its goal is to prevent severe disease, hospitalization and death rather than to eliminate infection entirely.
That doesn’t mean the COVID and flu vaccines are failures, health experts at Northeastern say.
Mansoor Amiji, university distinguished professor of pharmaceutical sciences and chemical engineering, and Neil Maniar, professor of the practice in public health, say vaccines differ according to whether the viruses they’ve been designed to quell are mutating or stable.
Stable versus mutating viruses
The measles and polio viruses are stable and don’t mutate over time, Amiji says. The same is true for the virus for smallpox, which has been eradicated globally and only exists in the lab.
Making a vaccine with an antigen from a stable virus means a vaccinated person’s immune system is primed to recognize and destroy the virus every time it appears, Amiji says.
“If you start to see an outbreak of polio, in any part of the world, these vaccines are still incredibly effective. If the virus crops up, it won’t evade the immune system or evade the vaccine’s response,” he says.
Such is not the case with influenza, the virus that causes flu, and SARS-CoV-2, the virus that causes COVID-19.
COVID-19 has gone through an alphabet soup of strains, from the Alpha to Beta, Delta, Omicron, Pirola and Eris — and is still evolving.
“Even though we have so many people either having natural infection or who have been vaccinated, these viruses continue to mutate,” Amiji says.
“We’re making vaccines that are looking for the spike proteins in the virus and are basically teaching our immune cells to look for the spike protein. But if the spike protein is mutating, then the vaccine efficacy starts to wane,” he says.
Influenza mutates even faster, which is why there are new flu vaccine formulas every year and why 50% is considered a good efficacy rate, he says.
The combinations of antigenic proteins on the influenza surface, known as hemagglutinin and neuraminidase — the H and N in virus nomenclature — vary year to year and even within the flu season, Amiji says.
The flu vaccine is “made up of a cocktail of these peptides,” he says. “It’s really a guessing game. There is no way of knowing which strain will be prevalent and which vaccines will work,” he says.
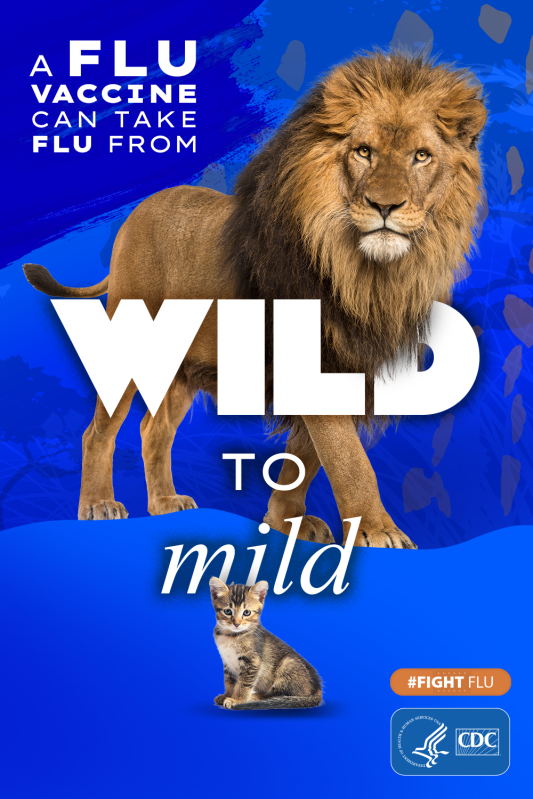
‘Wild to mild’ campaign manages expectations
That rate is making the flu vaccine a harder sell among the public.
The Centers for Disease Control and Prevention says during a year with a good match, vaccination reduces the risk of flu illness by between 40% and 60% among the overall population.
Consumer research shows “that many people believe flu vaccination doesn’t work because of first- or second-hand experience where vaccination may not have prevented illness,” the CDC says.
Concerned about drops in flu vaccination among high-risk groups such as pregnant women and children during the COVID-19 pandemic, the CDC this fall came up with a new campaign — one that spotlights how the flu vaccine can reduce not only the risk of influenza but of potentially serious outcomes.
Called “Wild to Mild,” the campaign pairs images of powerful and dangerous animals with innocuous counterparts — a raging bear with a teddy bear or a lion with a kitten, for instance.
“It’s definitely a change in messaging,” Maniar says.
“It’s a clarification in what is being messaged,” he says. “There has been sort of this prevailing idea that, ‘If I get the vaccine, I’m not going to get the flu.’ And we know that’s not the case.”
“There’s a lot of empirical evidence to show what the vaccine really does is it reduces severity. It reduces the likelihood that someone is going to be hospitalized or even die from getting the flu,” Maniar says.
The same is true with vaccination for COVID-19, he says.
“There are some individuals who after getting vaccinated will not get the flu or get COVID, because their immune systems have a more robust protection against the virus,” Maniar says.
“But that’s not the case for everyone. I think that’s where managing expectations comes into play,” he says.
The updated COVID vaccine — no longer called a booster by the FDA — targets the XBB.1.5 Omicron strain prevalent this spring. Pfizer says the monovalent vaccine also addresses currently circulating offshoots of Omicron, known as Eris or EG.5, and Pirola, BA.2.86.
“Vaccination remains right now our best strategy to not just ideally prevent but to have a benign type of infection, just basically a few chills and a sore throat,” Amiji says.
“It would be great if you don’t get infected. But even if you do get the infection it will be very mild, and you won’t be hospitalized.”
Improving the odds with universal shots
The flu virus undergoes both antigenic shifts and drifts, Amiji says.
The former is when hemagglutinin and neuraminidase undergo such huge changes the influenza vaccine is not effective at all. Drift is when slight modification occurs, he says.
There are glimmers of hope that both flu and COVID vaccines will become more effective in the future, Amiji says.
Using AI in pharmaceutical technology has led to preclinical studies showing the effectiveness of a universal mRNA flu vaccine that covers more than dozen flu strains in a season, he says.
“The same concept is being applied to a universal COVID vaccine,” Amiji says.
“They’re not in the clinic yet,” he says, but adds he wouldn’t be surprised if they were on the market by next fall.
In the meantime, Amiji says he plans to get the updated COVID vaccine and a flu shot this weekend.
“I would absolutely recommend that people get their flu and COVID vaccines as soon as possible,” he says.
“As we get toward the winter season, and people start congregating with Thanksgiving holidays and Christmas holidays, the propensity for infection just increases.”
Cynthia McCormick Hibbert is a Northeastern Global News reporter. Email her at c.hibbert@northeastern.edu or contact her on X/Twitter @HibbertCynthia.






