Will fall’s COVID vaccine protect against the emerging Pirola variant? When should I get the shot?
A new series of COVID vaccines is expected to be available in mid-September, leading to questions about how protective they will be against the latest variants and when people should get their shots.
Northeastern Global News talked to health experts at Northeastern about why they suggest waiting until October to be boosted and why the jury is still out on vaccine effectiveness against the latest variant to emerge, BA.2.86, also known as Pirola.
Latest vaccines based on variants circulating in spring
The Centers for Disease Control and Prevention says the updated COVID vaccine will be available in mid-September.
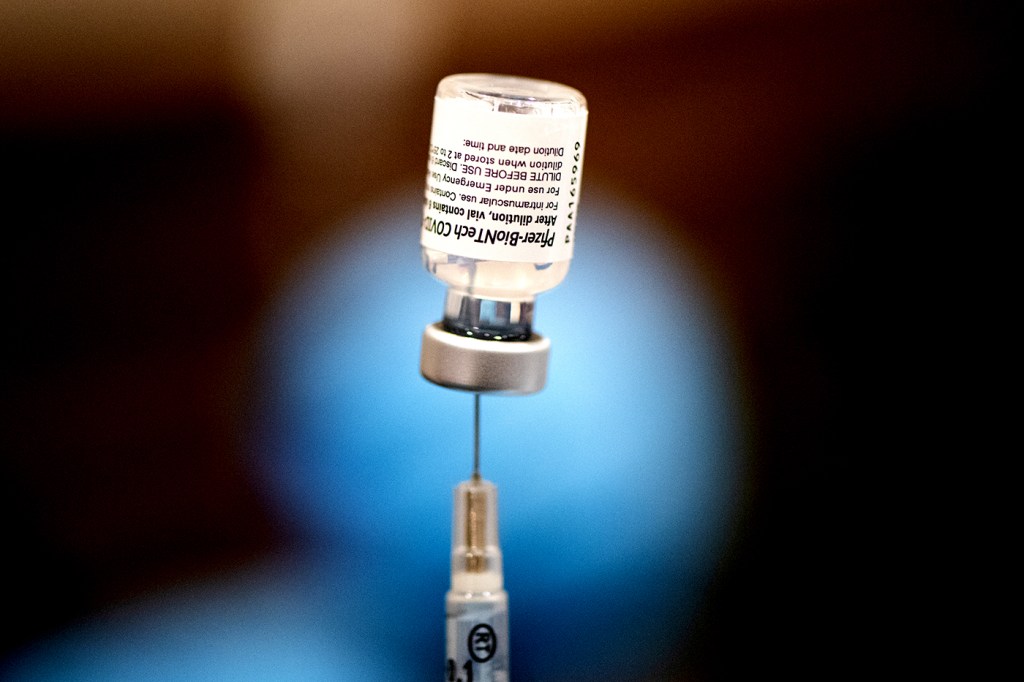
The Pfizer, Moderna and Novavax boosters are designed to protect against omicron subvariant XBB.1.5, which began circulating widely last fall and was the dominant strain this spring.
“We’re switching to a model where we’re going to have annual vaccinations in the same way that we have with the flu vaccine,” says Neil Maniar, director of the Master of Public Health Program at Northeastern.
And, as with the flu shot, focus is on developing a fall vaccine based on strains circulating in the spring.
But variants change, and now the dominant COVID variant is EG.5, known as Eris, which the CDC says accounted for nearly 21% of COVID cases in the U.S. in mid-August.
A descendent of omicron, Eris is named after the ancient Greek goddess of strife.
But so far it does not seem to be causing more severe illness than other omicron strains, which themselves were less severe than the original alpha and the delta variant, says Brandon Dionne, an associate clinical professor in Northeastern’s School of Pharmacy and Pharmaceutical Sciences.
Dionne, who also works at Brigham and Women’s Hospital, says patients currently hospitalized with COVID are much less likely to be seriously ill than at the height of the pandemic.
“Most people have been exposed in some way, either through vaccines or through infection, and have some level of antibody response so that even if they get infected, it should make (the illness) less severe,” he says.
“That’s really the goal of vaccines,” Dionne says.
New variant Pirola is a wild card
The vaccines being updated for fall should offer protection against Eris because they were formulated against a fellow omicron variant, Maniar and Dionne say.
Moderna announced in mid-August the preliminary clinical trial data showed its updated COVID-19 vaccine “showed a significant boost in neutralizing antibodies against EG.5 and FL.1.5.1,” which indicate it would “effectively target the expected circulating variants” this fall.
But the Pirola variant is raising concerns among health practitioners and scientists.
“This one seems to be different,” Maniar says. “There are many more mutations with this variant, which means that it will have a greater ability to evade the immunity that is conferred by vaccines and natural infection.”
“We’ll have to keep an eye on that,” Maniar says.
So far, caseloads of BA.2.86 or Pirola are low, but with more than 30 protein spike mutations, that could soon change.
The Pirola variant was first detected in August in samples from people in Denmark and Israel, the CDC says. At least two cases have been identified in the U.S.
The variant was found in a sample of U.S. wastewater, which the CDC says is being “closely monitored” for the spread of Pirola.
The federal health agency also is keeping track of hospitalizations that may arise from the new variant.
“It’s so new of a variant we don’t even know if it’s going to be more infectious or cause more severe disease,” Dionne says.
We’re switching to a model where we’re going to have annual vaccinations in the same way that we have with the flu vaccine.
Neil Maniar, director of the Master of Public Health Program at Northeastern
Should I wait until October for my shot?
While scientists evaluate the effectiveness of the updated COVID vaccines, the CDC urges people to get their shots this fall to reduce the risk of severe illness and hospitalization.
“It may not be as good as if we had a specific vaccine designed for that variant with its mutations,” but the updated vaccines should offer some decree of cross protection immunity, Dionne says.
While there was an uptick in COVID cases this summer, winter is when the illness typically spreads widely as people gather indoors and for holiday celebrations.
“COVID does not have the same seasonality as flu, where we see very little in the summer,” Dionne says.
“But it does seem to have a degree of seasonality where we do see more cases in the winter, which probably has to do with the increased risk of transmission,” he says.
To time vaccinations to achieve full effectiveness in advance of holiday gatherings that start in November, both Dionne and Maniar say people might want to wait to be vaccinated until later in October, just before Halloween.
It typically takes about two weeks to get a full vaccine response, although it may be shorter for a booster, Dionne says. “A week or two weeks is probably on the safer end to have that full antibody response.”
Combine with the flu shot or stagger shots?
Some people may wonder whether to get their COVID booster at the same time as their flu vaccine or whether to schedule them separately.
“We have data with the COVID vaccines and the flu vaccines that show they don’t seem to interfere with one another. So you certainly can get them at the same time,” Dionne says.
People tend to have milder reactions to the flu vaccine than to the COVID shot, which can trigger more of an inflammatory response, he says. For that reason, some people may want to space them out.
“It’s an individual decision for each person,” Dionne says.
He also doesn’t think it matters which arm is injected with which vaccine. Eventually, Dionne says, the plan is for “co-formulated vaccines” that deliver the flu and COVID vaccines at the same time.
Remember antivirals for COVID infections
People getting updated COVID shots have a choice of an mRNA vaccine from Moderna or Pfizer or a more traditional vaccine from Novavax that includes part of a spike protein plus an adjuvant that increases immune response, Dionne says.
Those falling ill with COVID likely will not have access to monoclonal antibody treatments that relieved symptoms and viral loads from the delta strain.
“We lost most of the monoclonal antibodies” during the omicron outbreak, Dionne says.
The FDA limited the use of the treatment in 2022, saying it wasn’t effective against omicron variants.
But Dionne says people who fall ill with COVID will still have access to the antiviral medications Paxlovid in outpatient settings and remdesivir in the hospital.
“They should work against this new variant” as well, he says.
Cynthia McCormick Hibbert is a Northeastern Global News reporter. Email her at c.hibbert@northeastern.edu or contact her on Twitter @HibbertCynthia






