‘Gut lab’ helps scientists understand the effects foods have on our bodies and improve drug delivery
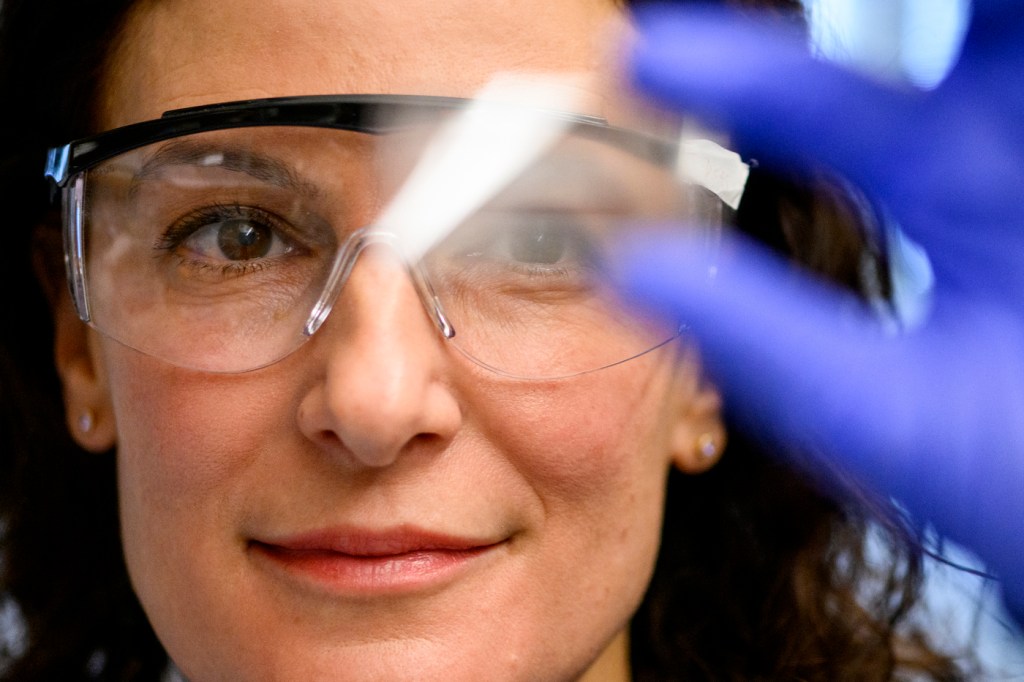
Professor Rebecca Carrier’s “gut lab” at Northeastern was born out of a big problem in the pharmaceutical industry.
It was not enough to develop a new active drug compound to bring a new cure to the market. Each drug needed a unique formulation that would allow the body to dissolve and absorb it, but there was no easy way to come up with such a formula in each case.
“One problem I saw as a formulation scientist was that a lot of what we did was trial and error,” says Carrier, associate chair for research in the chemical engineering department, professor of chemical engineering with affiliations in bioengineering and biology.
Usually, people prefer to take drugs orally rather than via an injection. But many drugs have very low solubility in the gastrointestinal tract or they don’t pass across the intestinal wall. Therefore, they can’t be delivered orally. Because of that, pharmaceutical companies sometimes abandon developing a drug because there might not be enough market interest for it otherwise.
Carrier decided to leave the industry and return to academia to find solutions.
“That problem prompted this whole big area of research that we do now,” she says, “what we call mechanistic studies and modeling of drug delivery.
Since she first joined Northeastern in 2003, Carrier has raised almost $20 million of external funding for her research; made pioneering advances in the drug delivery field; co-created a computational model capable of predicting oral drug absorption rate; invented a device used in cell culture research; and co-founded a company, MechaSim, that is focused on designing effective drug delivery systems for the pharmaceutical industry.
Her research at the Advanced Drug Delivery Research Lab has been closely related to the gut function which prompted her to seek gut models that could be used to study drug transport as well as mucus layer disruption with exposure to certain substances that may be present, for example, in food.
Someday, she hopes her research and practical work through MechaSim will give the pharmaceutical industry a tool that can help design drug products rationally, Carrier says, streamlining the resource-intensive drug development process and enabling oral drug delivery of compounds that might otherwise require injection. This tool will predict ahead of time how much of a drug will show in the patient’s blood if a delivery system is designed in a specific way.
“About 90% of what we do are benchtop experiments where we simulate the intestinal environment,” she says.
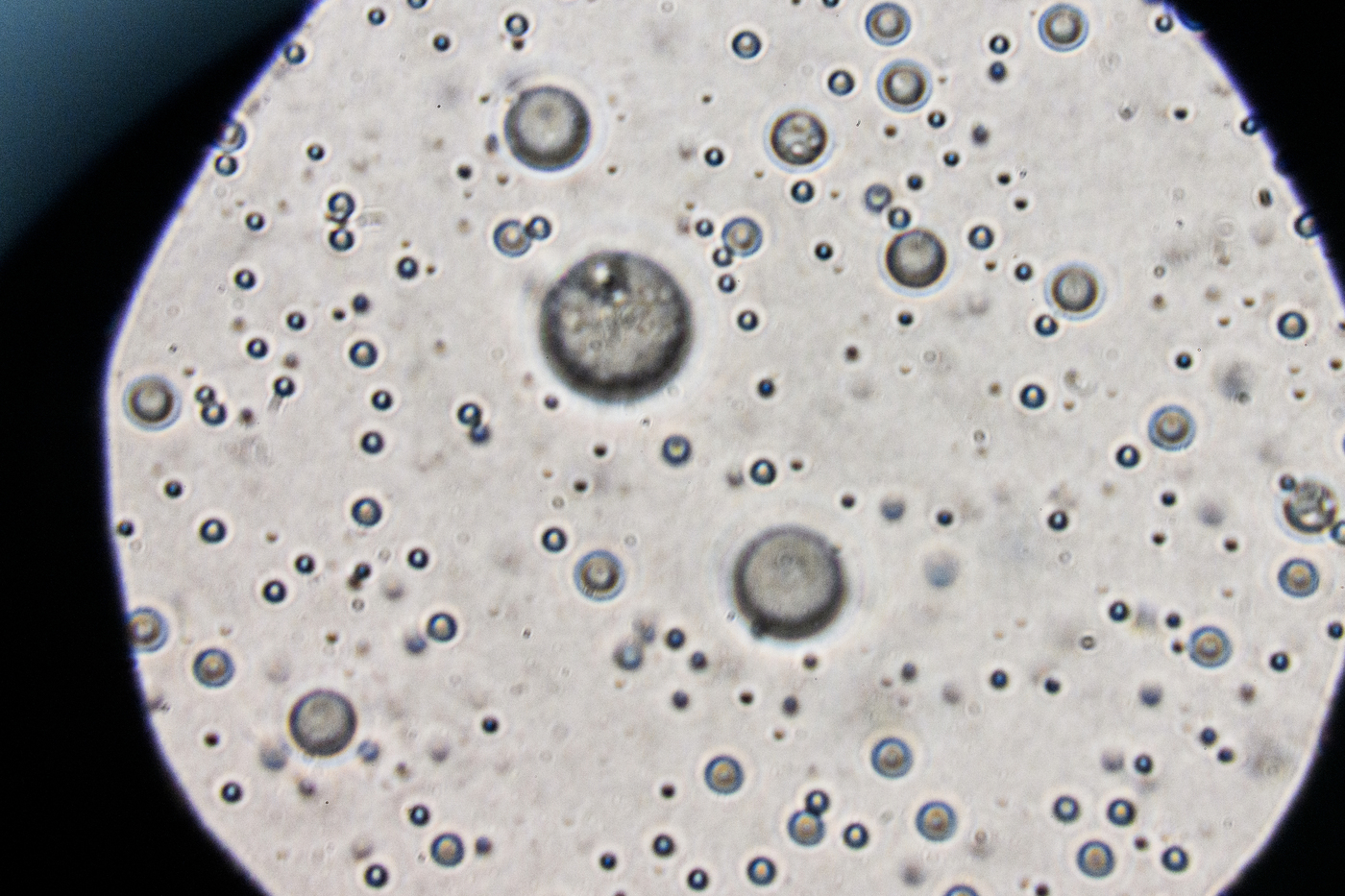
The mechanistic studies at the lab are usually done on solutions that simulate intestinal fluids. Such solutions consist of all the things that would be present in one’s gut, like digestive enzymes and bile components. That allows scientists to study different processes like drug dissolution during simultaneous digestion of other intestinal contents.
The Advanced Drug Delivery Research Lab especially focuses on lipids, which are used a lot in drug delivery systems and also present in our food. Lipids (fatty acids or their derivatives) can have a drastic effect on the way compounds are absorbed by the body, but the scientists don’t yet fully understand the underlying mechanisms and cannot predict how much of a drug will show in the blood when dosed with a certain amount of lipid. To address this challenge Carrier’s lab studies drugs in simulated intestinal environments with lipids and observes how they affect drug dissolution and partitioning.
She is also fascinated with mucus, which lines the GI tract and other wet epithelial surfaces.
“It is the first barrier for most things getting into the body,” Carrier says. “What isn’t really well understood is how much of a barrier is mucus to drug delivery.”
She is interested in how the mucus barrier changes with different conditions and how these changes might relate to disease.
“For example, with exposure to lipids in the GI tract, it turns out that the mucus barrier changes a lot, and that might explain why sometimes we see really strange effects with certain drug delivery systems with a fed state versus a fasted state,” she says.
Carrier’s hypothesis in a wider sense is that mucus layer disruption is an underlying mechanism of inflammation in the gut, which is tied to many different health conditions.
“A high-level goal [for the lab] would be to demonstrate that this is a mechanism because then it makes the mucus layer a new therapeutic target that people haven’t really been thinking about,” she says.
Carrier believes that disruption of the mucus layer might be easier and more accessible to address than much more complicated issues with cells.
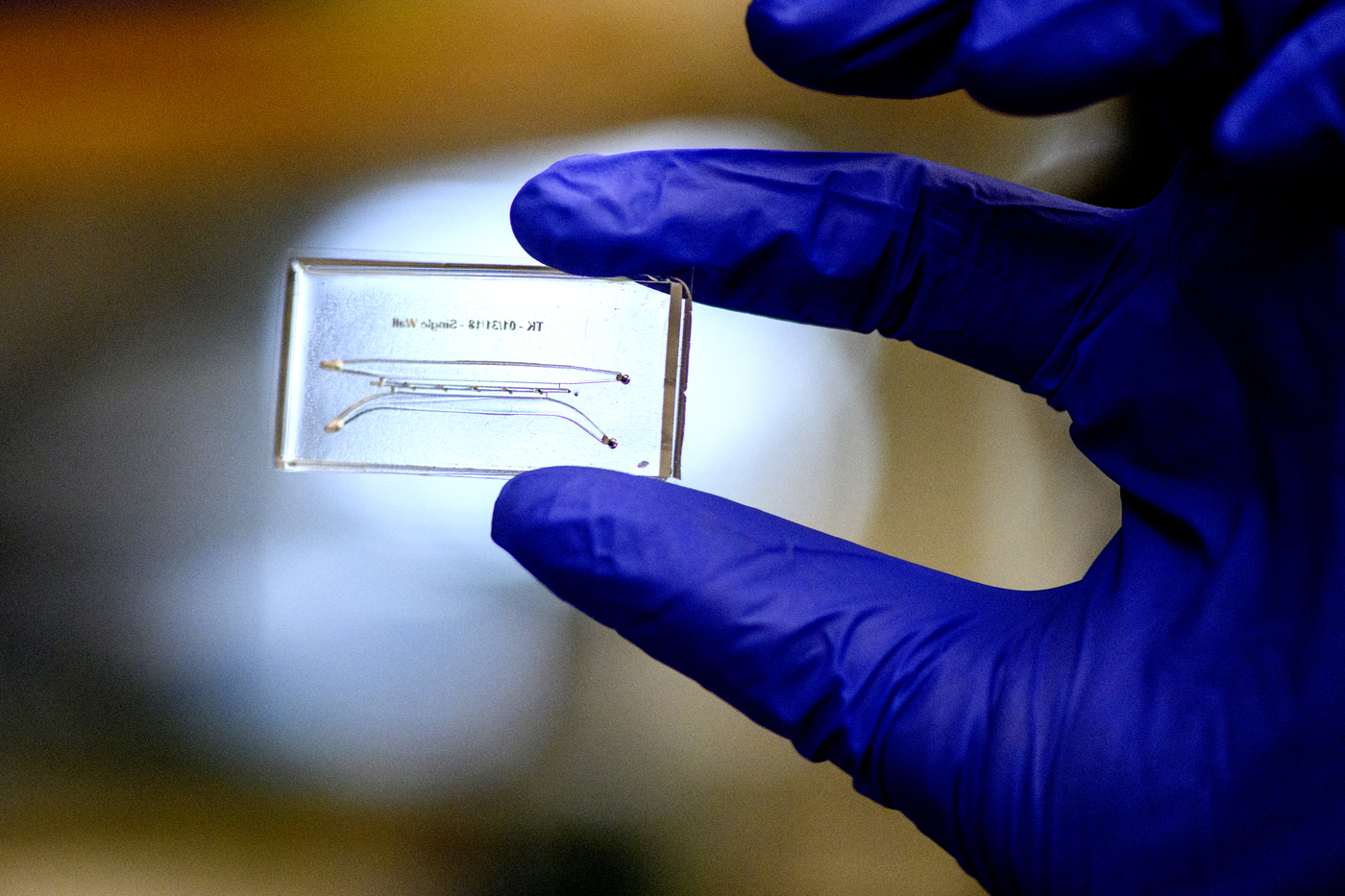
These aspirations lead to the third area of the research at the Advanced Drug Delivery Research Lab—development of gut-on-a-chip systems.
To study mucus secreted by intestinal cells, the lab worked with collaborators at MIT to develop a 3D-printable polymer model of a gut that can hold gut epithelium, bacteria representative of microbiome and immune cells. The gut-on-a-chip looks like a little slide with channels that represent lumen (the inside of the GI tract) and circulatory system, or lymphatic system. The epithelium grows on a vertical wall within the device so that mucus is easily visualized using a microscope.
“We’re trying to demonstrate, using our gut-on-a-chip systems, that when you add things which are known to disrupt the mucus layer you see an inflammatory response,” Carrier says.
The gut chips could also be used in the future for studying the effects of different food substances which are associated with disease or could represent nutritional interventions.
The lab does a lot of work in collaboration with industry, Carrier says. For example, currently they are working with such biotechnology and pharmaceutical companies as Genentech and AbbVie, who seek to understand the significance of the mucus barrier.
“I feel really blessed to be working on what I think are really fun and important problems,” she says, “as well as working with students and collaborators who are amazing.”
Alena Kuzub is a Northeastern Global News reporter. Email her at a.kuzub@northeastern.edu. Follow her on Twitter @AlenaKuzub.






