Who gets a COVID-19 vaccine first–and how do you decide?

A third potential COVID-19 vaccine emerged on Monday, with pharmaceutical company AstraZeneca joining Moderna and Pfizer in announcing promising results from early-stage clinical trials. As the companies jockey for emergency use authorization from the U.S. and other countries, a new question has emerged: If the vaccines are approved, who gets a dose first?
The first step should be to establish a shared set of values, rather than target specific populations, according to Mark Wells, a visiting lecturer of philosophy who studies how ethical theories can inform public policy. The second step, says Wendy Parmet, Matthews Distinguished University Professor of Law, “is figuring out a way to implement a plan without stumbling over existing inequities.”
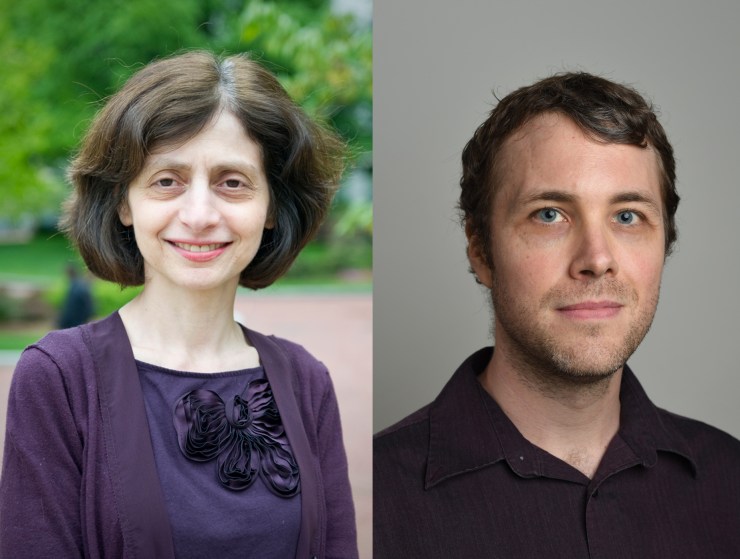
Wendy Parmet, left, is Matthews Distinguished University Professor of Law and director of the Center for Health Policy and Law. Mark Wells, right, is a visiting lecturer of philosophy. Photos by /Northeastern University
And there’s broad consensus among biomedical ethicists, he says, on a handful of such values.
“We should be worried about preventing people from dying from diseases and about fair and equitable distribution of resources,” Wells says, “as well as being committed to respecting people and facilitating a high quality of life for people.”
These values—mitigating harm, equality, honesty and respect, and general welfare—can then be used as a framework within which to hammer out the specifics, he says.
In the U.S., the members of president-elect Joe Biden’s COVID-19 task force will be some of the architects of these dynamic frameworks and their details, and there is already some indication of how it might play out, Wells says.
Biden’s team includes Zeke Emanuel, a former Obama administration healthcare advisor, whose past work gives insight to his priorities when it comes to a COVID-19 vaccine.
“In the past, Zeke Emanuel has focused on limiting harms, prioritized the disadvantaged, and put a high value on recognizing the equal moral worth of everyone,” Wells says.
Emanuel has articulated a framework in which frontline healthcare providers—people who perform high-risk essential activities that keep society running—will be among the first in line, he adds.
Prioritizing frontline medical workers could save more lives in the long run, Wells says. Keeping emergency and medical workers healthy and active allows them to treat other people.
Once a plan is in place, however, a new challenge emerges, says Parmet, who is the director of the Center for Health Policy and Law.
“The second challenge is figuring out how to implement it in a way that does not stumble over existing inequities,” Parmet says Parmet.
If mitigating harm means prioritizing healthcare workers, older people, and people with comorbidities, “the essential concern is: How do you actually find those people?” she adds.
Elderly people who live outside of nursing homes, are undocumented, speak languages other than English, or don’t have health insurance or access to the internet, are all at risk of being left out of a widespread vaccine distribution program, Parmet says.
“We need to make sure that the way you get access doesn’t create its own roadblocks,” she says.
For media inquiries, please contact Shannon Nargi at s.nargi@northeastern.edu or 617-373-5718.