‘We find ourselves asking scientists to do more than simply study the coronavirus’
As the COVID-19 pandemic evolves, epidemiological models continue to provide vital information for lawmakers, public health officials, and individuals trying to slow the spread of the virus.
This has put the modelers conducting this research in the spotlight. And accurately communicating these data and insights to the public has been a challenge.

“We find ourselves asking scientists to do more than simply study the virus,” said Mark Patterson, associate dean for research and graduate affairs in Northeastern’s College of Science, in a conversation streamed on Facebook Live. “In state houses, in cable news interviews, and on social media, they’re translating their data into insights, recommendations, and even advocacy.”
Patterson spoke to Samuel Scarpino, head of Northeastern’s Emergent Epidemics lab, to discuss how science is being communicated during this pandemic. Scarpino has been working on modeling the coronavirus since January and has been sharing his insights with lawmakers, community groups, and news anchors for months.
“We are providing information, data points, model forecasts, to aid and support decision making—we are not making policy recommendations,” Scarpino said. “That is not the role of these models. It’s not the role of the mathematical epidemiology that we do. It is to paint a picture and provide the resources that are necessary for the policymakers to make the decisions around how they want to move forward to best protect their populations and also try to support the economy and ensure that individuals have the health services that they need.”
Your research has concluded that we as a nation were too slow to act in curbing the spread of the virus. Do you believe the policymakers and the public were not ready to hear the science behind COVID-19, or that the scientists themselves were not prepared to communicate? Or was it a mixture of both?
There were certainly a lot of complexities early on in the pandemic that led to the slow response in the United States and many other countries. One aspect was certainly because this was a novel disease. We were learning about the biology, the sociology, in real time, as the outbreak started to unfold. That’s one of the reasons why the messaging around things like face mask wearing has changed, because our understanding of the importance of that type of intervention has shifted.
However, when I think back to early February, March, it was very clear that the disease was spreading rapidly in China, that it was starting to move out of China into surrounding countries. We were starting to see early cases in the United States. And that was the opportunity to ramp up testing, and to focus on testing individuals who met the case definition, meaning the symptoms that are associated with COVID, as opposed to just focusing on travel history.
So what we saw, retrospectively, is that a number of early introductions on the West Coast—Seattle, California—were stopped with public health measures. We identified the cases, we performed contact tracing and isolation, and we prevented the outbreak from taking hold. However, once the pandemic was seeded in Europe, and we started having cases come into the eastern United States, we were no longer finding those individuals because we had both a low capacity to test and we were focused heavily on China, and were missing those individuals that were traveling through Europe in the United States.
In a situation like this, do scientists need to become advocates for using data, if policy issues or if government organizations are either unwilling to understand the message or unwilling to implement the necessary health measures? Is it fair to ask scientists to be advocates?
I think it’s certainly an expectation that scientists should have of themselves that if there is an opportunity and a need to advocate on behalf of the research that you’re involved in, then those kinds of advocacy methods or approaches are important.
However, it’s impossible for almost anyone to be an effective advocate, an effective communicator of science, overnight. And so one of the things that we’re seeing as an increasingly important part of scientific training is ensuring that individuals have the science communication training, the advocacy training, but importantly that they have the support network around them, because most of us are not, and will not ever be, experts in public policy, in advocacy, in science communication.
I think you really have to be building that skill set and building those networks of collaboration before the pandemic hits, so that you’re not trying to implement all this as you’re also learning about a new disease and trying to stop it in its tracks.
The United States is significantly behind other countries and we’ve got very lax and uneven state policies with regard to managing the health aspects of this crisis. Do you think we really need a command and control at the national level to deal with something at the scale of a country? Are you an advocate for national control as opposed to regional, state-level measures?
One of the challenging aspects about the COVID-19 pandemic has been the essential absence of leadership at the federal level. So we know that the CDC has really not been a daily feature as they were in 2009 with H1N1, in 2015 for Ebola, and with Zika virus as it was hitting our continent. And so that sort of void is also part of the reason why many scientists have had to step up into these advocacy and public policy roles–because the traditional venues where that advocacy is communicated, where the science is translated into policy, have not been available.
And what we’re seeing is the need for federal coordination when it comes to implementing things like mask-wearing, testing, approving testing, determining what are safe and effective measures for keeping cases from growing into large local epidemics.
All that being said, of course, you think back to April, as Boston was experiencing one of the largest surges of COVID-19 in the globe, there were parts of the U.S. like Arizona, Texas, Florida that were not seeing very large outbreaks. And now, of course, things have flipped and Boston is continuing to see day over day, week over week, declines in cases while they’re spiking in Arizona. And so we need a system where there’s federal-level coordination, but also flexibility at the local level to respond to differences in what’s happening in people’s neighborhoods.
I wonder if you could tell us a little bit of the modeling approaches you and your team have been taking. For example, how do you scale up from helping the mayor of Boston, to then helping the governor of Massachusetts, to then helping the regional group of governors in New England, manage something of this magnitude?
The first step that we took from the modeling approach was to begin building large scale data sets around COVID-19. One of the things that we know from past outbreaks, from past pandemics, is that it’s very difficult to get high-resolution, accurate, validated data, especially early on during a pandemic to power those models that we’ve been seeing across the front page of The New York Times and The Washington Post.
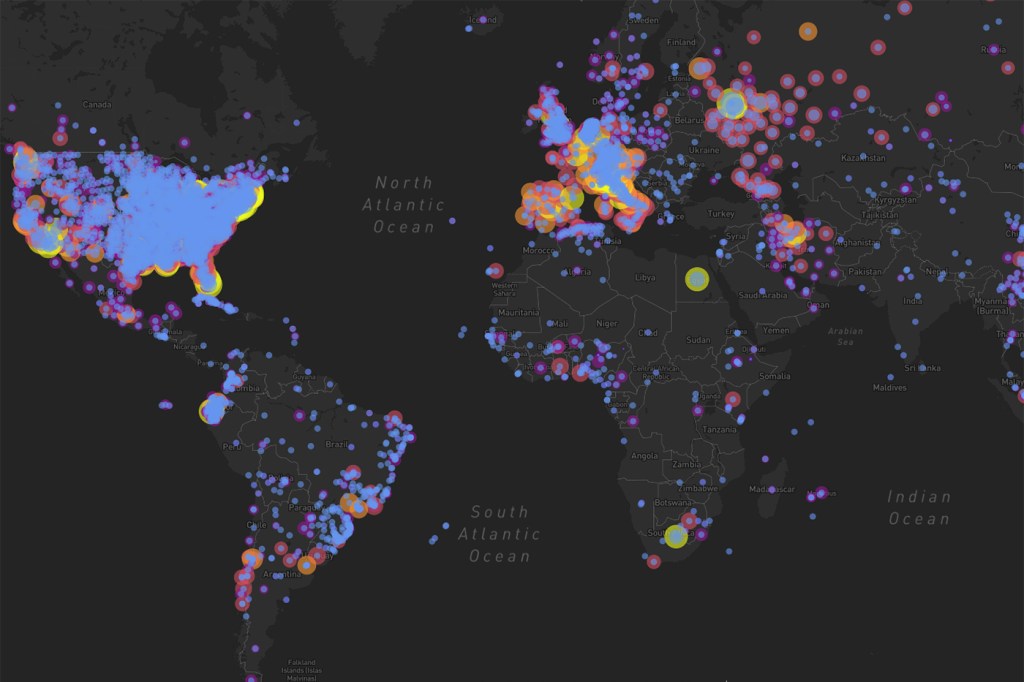
So we stood up a volunteer consortium across the globe, institutions like Oxford and Beijing Normal University, Northeastern, University of Washington, collaborating with technologists at Boston Children’s Hospital, Healthmap, Mapbox and now Google to build a comprehensive data set around COVID-19 to power these mathematical models.
In terms, then, of actually scaling, part of that scaling is the preparation ahead of time. Researchers at Northeastern University like Alessandro Vespignani and the MOBS lab have been building towards COVID-19, in terms of their response to past outbreaks, for decades. And so they have the computational infrastructure, they have the political experience in terms of navigating the various state, federal, international organizations, to be able to rapidly deploy these kinds of tools. So it’s a combination of building the data sets and tailoring the models to the specific policy questions that affect Boston, affect Massachusetts, affect the United States, affect our global community, but then also having the frameworks and foundations in place so that you’re ready to deploy even before the pandemic happens.
Tell us a little bit about the open source data essentially crowdsourced from your community of scientists and medical experts out there. And why would this data not be available already with modern healthcare systems?
Why the data would not be available is the kind of question that would require essentially a dissertation to fully answer.
Why isn’t the World Health Organization able to collect and share epidemiologic data? It’s part of their mandate, but they have to negotiate with all of their member states, many of whom barely get along with each other, and all of the data-sharing agreements, the collection, what can and can’t be accessed by whom and for what has to be negotiated. And typically it has to be negotiated as the pandemic is unfolding. We saw this during Ebola, we saw this during H1N1, we saw this during Zika and chikungunya.
So we were anticipating the complexities around data-sharing by these nongovernmental organizations or government organizations like the CDC—a similar kind of complexity, in terms of data sharing as it interfaces with politics, affects the CDC’s ability to share information from state and local health agencies across the United States.
However, what has changed since 2009 is that vast amounts of health data, epidemiologic data, are reported through news sources, through public channels, coming out of state, county, and city health departments and national health departments.
And so two individuals in particular—Moritz Kraemer, who’s a research fellow at Oxford, and David Pigott, who is an assistant professor at University of Washington—realized that we needed to begin entering these data ourselves into an open source comprehensive database. And those individuals grew to what is a team of now over 100 people. We’ve entered about 2 million individual records from 150 countries. We have brought on engineers from google.org to help us scale the technology and computational infrastructure behind the data. We brought on brilliant designers and product managers.
We’re rebranding ourselves under this new kind of international consortium, of which Northeastern is a major part, to not just provide data for COVID-19 over the coming weeks, months, and probably years, but also for the next pandemic that we know is coming in the future.
What’s your read of the national situation with respect to what your models are predicting? What’s in store for the fall and how does aerosol transmission, transmission just through being in the same airspace as somebody, figure into this as we go back to work?
Part of the reason the lockdowns were so important is that we needed to make sure that the entire country doesn’t synchronize with respect to COVID, because then all of the healthcare systems will be overwhelmed at the same time, which is what we were doing with the ‘flatten the curve’—preventing the healthcare systems from being overwhelmed.
And so we were very aware of the likely scenario that we would see outbreaks in New York City, Boston, the East Coast, the places that had the first cases. And then we would likely see outbreaks in other large cities in the U.S. and comparatively more suburban and rural areas later into the summer. And so this kind of pattern is almost exactly what we were expecting with, of course, variability in terms of magnitude in the predictions.
We know that mask-wearing is highly effective at stopping transmission. We now know that probably 80 percent of transmission events result from 10 or 20 percent of people that are infected. And so a combination of reducing gathering sizes and mask wearing will dramatically slow down COVID-19. So when we see states like Arizona, Texas, Florida, opening up, having large gatherings, not enforcing mask-wearing, given that they hadn’t had an outbreak yet, it’s essentially a perfect storm for generating the kinds of massive waves that we’re seeing now.
Now, the question around the fall is one that’s very, very hard to answer. It’s really going to depend on mask-wearing. It’s going to depend on what decisions are made around how to reopen different parts of our society. It’s going to depend on how this coronavirus will interact with influenza—that’s something that we don’t know very much about for this particular coronavirus.
It’s going to depend on the specifics of how transmission works, in terms of our social network structure. That affects quite a bit where the herd immunity threshold, which is the fraction of individuals that have to be immune for there to be a low chance of an outbreak turning into an epidemic, is.
These are all questions that we’re learning right now, and still don’t have a great answer for.
For media inquiries, please contact media@northeastern.edu.





