When healthy habits become risky business
“When people take precautionary measures, their behavior often changes as a result,” said Ravi Sundaram, an associate professor in the College of Computer and Information Science at Northeastern University. For example, people wearing seatbelts may drive faster, people who’ve received flu shots may skip washing their hands before eating, and those who’ve been vaccinated against sexually transmitted diseases may tend to engage in more risky behavior.
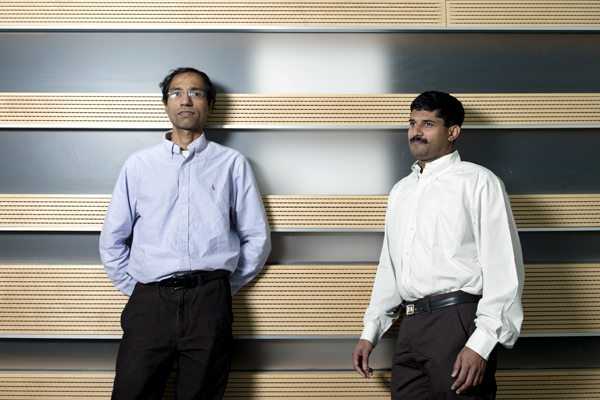
But how do these behavioral changes affect a contagion’s spread when the precaution is not foolproof? This is precisely the question that Sundaram and his colleague, professor Rajmohan Rajaraman asked in research recently published in the Journal PLOS ONE.
The duo used network science techniques to look specifically at the influenza vaccine, which has a 20 to 40 percent chance of failing, and the HIV/AIDS antiretroviral, which is unsuccessful 25 to 75 percent of the time.
Given these statistics, Rajaraman said, “if the level of risky behavior exceeds a certain threshold, then you arrive at some strange scenarios in which the more you intervene the worse you’re making it.”
The flu virus only requires that one person make a poor decision before it jumps to another host. In this case, if the vaccination rates are low, then increased vaccination will tend to make the problem worse. This anomaly does not occur, however, when a large fraction of the population is vaccinated, which will outweigh the negative impacts of risky behavior.
However, things aren’t this simple with STDs, which require two parties’ participation to be transmitted from one host to another. Here, risky behavior is overcome by increased vaccinations—but only to a point. Using a computational model based on data from the New River Valley in Virginia, the researchers found that after about 40 percent of the population was vaccinated, the tables turned. Now the risky behavior outweighed the positive impacts of the vaccine.
“What happens in the HIV case is that since the risky behavior requires consent on both sides, the number of risky interactions for low levels of vaccination is still very small,” said Rajaraman. “So you benefit with increased vaccination. But this may no longer hold at high levels of vaccination.” That is, one person’s risky intention will not translate into risky behavior until the second party is also vaccinated.
The critical takeaway of the research, Sundaram said, “is that we have to have some kind of behavioral intervention that is coordinated with the medical intervention. So we tell people go get a flu shot, but then you also need to accompany it with some kind of behavioral intervention in which you tell people to be aware that it isn’t perfect.”
The research is part of an ongoing collaborative study with computer scientists at Virginia Tech and epidemiologists at Pennsylvania State University in which the team is looking at similar problems across a variety of contagions.
The results, if confirmed in real-world settings, could have significant policy implications, said epidemiologist Stephen Eubank, one of the team’s collaborators at Virginia Tech University.





