Using technology to save the healthcare system
 The nation’s healthcare system is facing a financial crisis. It’s not big news. We’ve all known it for years. The planet (and the economy) is struggling to accommodate the largest population it’s ever had in a time when people are living longer than ever.
The nation’s healthcare system is facing a financial crisis. It’s not big news. We’ve all known it for years. The planet (and the economy) is struggling to accommodate the largest population it’s ever had in a time when people are living longer than ever.
“Everyone agrees that something needs to change, but how it will change no one knows,” says associate professor Stephen Intille, who has joint appointments in the College of Computer and Information Science and the Bouvé College of Health Sciences. Most health care professionals agree that preventive medicine will be a large part of the solution, but developing the business models to make it happen will be more complicated.
Intille represents a growing group of researchers merging the computer and health sciences hoping to make preventive medicine easier and more viable as a healthcare approach. Traditionally so-called “health informatics” tools have been “physician facing.” They allow physicians to acquire, store, retrieve, and use patient information via a broad range of technology applications. In it’s current incarnation, health informatics make things simpler for doctors when sick patients come to their offices.
While this works great for a “sick-care system,” Intille points out, it doesn’t do much in a “well-care system.” As such we need to rethink the field entirely. Intille and his colleagues in the new Personal Health Informatics (PHI) program are developing tools that patients can use in their home and daily life to promote healthy living.
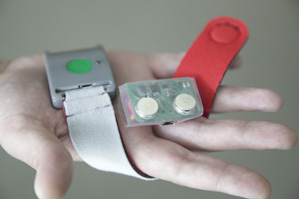
We’re not talking about the magnets that yell at you every time you open the refrigerator door. PHI devices are either entirely passive, collecting data about your movements and habits without your paying attention, or use positive feedback to reinforce good behaviors.
PHI tools can also reduce the cost of healthcare by lowering the overhead required to carry out research into various sick patient groups as we attempt to design better treatments. For example, assistant professor Matthew Goodwin develops tools to help treat and diagnose autistic patients in a more efficient and economical way.
Associate professor Timothy Bickmore develops virtual coaches to intervene across the spectrum of health care — from preventive medicine, to outpatient care, to in-hospital care, to the transition home. “Heath behavior is responsible for a very significant chunk of the health care burden in the US,” he says. This means that both taking care of ourselves before we get sick and then doing the things we need to do when we are sick are both extremely important.
And both can be addressed through PHI devices. Northeastern’s new PhD program attracts students from the health care field who are interested in using technology to deliver better care, as well as technology specialists interested in health and wellness.”There are 30 plus masters and doctoral level programs in health informatics in the US,” says Goodwin. “All of them are within managed care or electronic medical records, developing tools to assist physicians. What distinguishes this program is that it’s about creating technology for the person who is getting ill or is ill.”
…Or preventing the well from getting ill in the first place.
Photo by Jonathan Williams, MIT Media Lab





