A miniature device with a big impact
Ten milliliters of blood may not seem like a lot, and coming from healthy individuals it isn’t. But for critically ill patients with diminished resources, 10mL could be crucial. Nonetheless, that’s what’s currently required to test for circulating tumor cells in late-stage cancer.
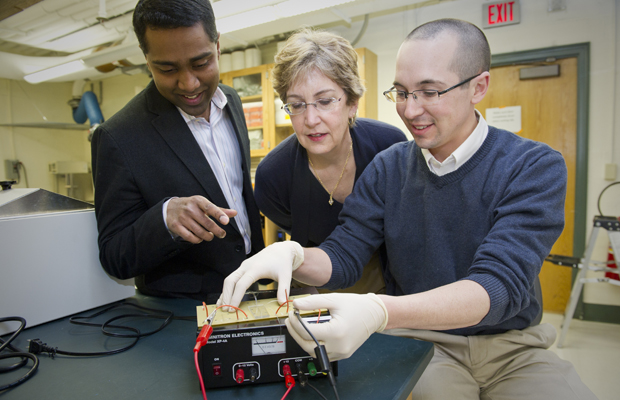
In a recently completed graduate thesis, Brian Plouffe employed the combined expertise of faculty members Shashi Murthy and Laura Lewis in Northeastern’s Department of Chemical Engineering to develop an alternative testing method.
Diagnosing metastasis in late-stage cancer patients requires identifying foreign cells in the bloodstream, known as circulating tumor cells. The current method for doing so involves a costly, inefficient technique called magnet-activated cell sorting (MACS).
As the name implies, clinicians tag the cells of interest with microscopic magnetic beads and then use a large magnet to separate them from the rest of the blood sample. The whole procedure, which first requires a lengthy sample cleanup process, takes place in a test tube and uses up the entire sample in one run.
Plouffe’s approach shrinks the process to a fraction of the size and cost. The method allows clinicians to pass a single milliliter of whole unprocessed blood through a miniaturized version of a MACS device, which can be tuned to test for a variety of cell types.
In the first two years of his investigation, Plouffe “described the whole thing with equations,” says Murthy. They started with extensive calculations that predicted how a particle would move in a magnetic field with a fluid carrier.
“We took a mathematical approach first before coming in and trying to build something that may or may not work,” Plouffe said.
Whereas Murthy afforded insight into the fluid dynamics part of the equation, Lewis’ expertise in rare-earth magnets and electromagnetism helped Plouffe determine how those elements would affect the system. “I don’t do bio,” Lewis said. “Shashi doesn’t do magnetism. But at the time Brian was still in the learning mode of both fields. He forged the collaboration in order to come up with something new that combined them.”
In January, the team published its first proof-of-concept results. They first fabricated the devices and then tested them with blood samples containing a known concentration of magnetically tagged breast cancer cells. The devices recovered up to 95 percent of the cancer cells with minimal non-target blood cell contamination.
Not only is Plouffe’s approach efficient and inexpensive, it is also portable and extremely user friendly. Plouffe imagines that it could one day be used in the field in underdeveloped nations to diagnose disease in real-time.
Murthy expects the device to have far reaching applications, with the potential to make early-stage diagnoses from a variety of fluid types (saliva, lymphatic fluid, etc.), and testing for cell types beyond cancer.





