A partnership to cure sleeping sickness
African sleeping sickness, which currently affects 30,000 people, starts out like the flu. Patients complain of fever, headaches and joint pain. But if Trypanosoma brucei, the parasite that causes the illness, remains in the body long enough, it infiltrates the central nervous system and becomes fatal.
As its name implies, sleeping sickness occurs exclusively in sub-Saharan Africa, where Tsetse flies carry T. brucei and where the population is generally too poor to warrant interest from major drug development ventures.
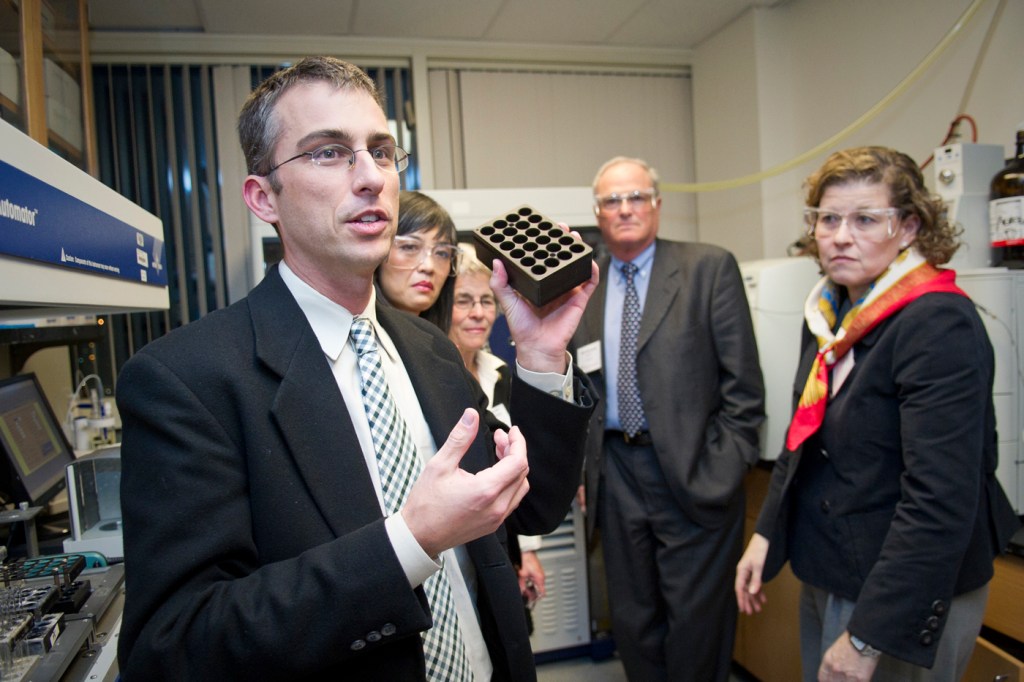
Michael Pollastri, an associate professor of chemistry at Northeastern, has joined forces with the Open Lab at GlaxoSmithKline (GSK) and Spain’s National Research Council for Scientific Investigations (CSIC) to identify new treatments for the disease. The collaboration, initiated by Pollastri and co-principal investigator Miguel Navarro of CSIC, employs a high-throughput screen of 30,000 pre-existing GSK kinase inhibitors for their effectiveness against T. brucei.
The work dovetails with Northeastern’s focus on use-inspired research that addresses global challenges in health, security and sustainability.
The symptoms that develop in stage I of sleeping sickness subside after a few weeks, and most patients do not receive treatment until they begin displaying the neurological symptoms that result when the parasites have invaded the brain (stage II). Because of this, Pollastri explains, “people are generally diagnosed when they’re in trouble, and then only with a spinal tap.”
The drugs that treat stage I are effective and not extremely invasive. But the existing therapies for stage II are lengthy, toxic and sometimes even fatal themselves.
“The central nervous system,” Pollastri says, “has evolved nicely to protect the brain.” As such, developing drugs that can get through the so-called “blood-brain barrier” into the central nervous system can be extremely difficult. But this is exactly what’s required to treat stage II sleeping sickness patients.
Pollastri’s collaboration, which crosses national and institutional boundaries alike, was approved for one year of funding from the Tres Cantos Open Lab Foundation (TCOLF). TCOLF provides funds so that external researchers can come to GSK´s R&D center in Tres Cantos (Spain) to pursue their projects as part of a drug discovery team and to tap into GSK´s resources and facilities.
“The compounds in a drug company’s files are predominantly drug-like,” Pollastri says. “The structures are such that you can modify them pretty quickly, and as a result are an attractive starting point.”
The high-throughput screen, which commenced in Spain earlier this month, will identify compounds of various potencies. Those that show promise will be pushed through a validation and optimization process. New, slightly tweaked versions of the GSK compounds will be funneled back through the screen. Ultimately, Pollastri hopes, this process will lead to drugs that can treat sleeping sickness with very few side effects.
Pollastri, who is heading up the new Neglected Diseases Initiative in the College of Science, is also spearheading other “target repurposing” studies, both in his lab here at Northeastern, as well as in collaboration with several other universities and institutions throughout the country.
View selected publications of Michael Pollastri in IRis, Northeastern’s digital archive.





