To fix health care, competing interests need to collaborate
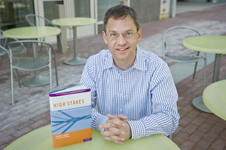
Greater collaboration among health-care stakeholders, including insurers, physicians and employers, could cure the United States’ ailing health-care system, according to a new book coauthored by Eric D. Kupferberg, of Northeastern’s College of Professional Studies (CPS).
“High Stakes: The Critical Role of Stakeholders in Health-care,” published in May by Oxford University Press, grew out of six years of research with health-care leaders, including junior executives of pharmaceutical firms, directors of public hospitals and benefits managers of Fortune 500 companies.
“The benefits of stakeholder collaboration hold true under a single-payer system or under a completely consumer-driven health-care system,” says Kupferberg, a senior assistant dean for academic and faculty affairs in CPS, where he directs the master of science program in regulatory affairs for drugs, biologics and medical devices. “My hope is that it spawns a healthy debate.”
Rather than collaborate, health-care stakeholders currently compete with each other in unrelenting fashion. “You could chart the competition and inefficient struggle between stakeholder groups,” says Kupferberg, “and each would have a hostile attitude toward at least three others.”
Take, for example, the contentious relationship between physicians and health insurers, who blame each other for the high cost of health-care and compete for every dollar.
As Kupferberg puts it, “Doctors view each dollar that a health insurance company makes as one less dollar that they need, but insurers who pay physicians think of it as one less buck that they make.”
Employers and employees are engaged in a similar debate over health insurance premiums, which tend to increase or decrease in concert with physical wellness.
Diabetes, and high blood pressure and cholesterol levels among employees contribute to the health-care costs of even the most profitable industries, according to Kupferberg, who says, “Overweight employees cost companies a fortune.”
The solution, he says, is company-wide health programs, in which employees who stay in shape pay lower premiums. “If an employee can demonstrate he has maintained a healthy weight, quit smoking and followed disease management principals, then an employer might reduce his premiums,” says Kupferberg.
He suggests that hospitals that agree to take an evidence-based approach toward diagnosing and treating patients could receive more reimbursement money from health care providers. The strategy, in turn, he says, could “increase the quality of care, while reducing cost.”
Politicians may begin asking Kupferberg for advice on fixing health-care. “I expect to be invited into the fray,” he says.





