Published on
Cystic fibrosis is difficult to treat. Computer modeling may hold the answer
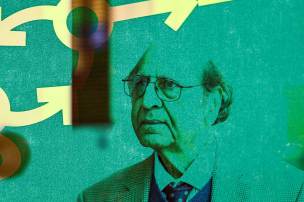
Northeastern professor Srirupa Chakraborty’s lab uses high-powered computing to develop proteins with a range of possible uses, from water purification to more effective drug treatments for a range of stubborn diseases.

Treating cystic fibrosis has long confounded the medical community because of the combination of what it does and where it tends to do it within the body. The incurable genetic disorder, which the American Lung Association estimates affects nearly 70,000 people worldwide and shortens life expectancy to between 40 and 50 years old, works by mimicking the body’s natural defense mechanisms — in this case, overproducing a thick mucus that coats vital organs and the lungs in particular.
Normally, the lungs have a natural mucus defense barrier against pathogens, called a mucin layer. By thickening it, cystic fibrosis both hampers organ function and prevents therapeutic drugs — like nasal sprays — from getting through effectively via conventional delivery methods for lung afflictions. Other conditions, including gastrointestinal inflammation, rheumatoid arthritis and certain cancers pose similar problems.
In recent years, innovative new treatments for the disease have emerged, including mRNA-based gene therapy. But many forms of medicine “get stuck in that mucus layer, and therefore the drugs are not being delivered correctly,” says Srirupa Chakraborty, a biophysicist and Northeastern professor in chemistry, chemical biology and physics. “And bodies are now more susceptible to infections, because that mucinous layer has changed.”

Chakraborty’s SymBioSys Lab is working to solve that delivery problem. And the researcher, whose resume includes stints at IBM’s Watson research center and Los Alamos National Laboratory, where she investigated the molecular structures of HIV and COVID-19, says Northeastern is uniquely set up to help her do it. That’s because her lab doesn’t use medical equipment or clinical trials. Instead, her team designs and simulates the function of special biomaterials that can serve a broad range of potential purposes, from drug delivery to water purification, through computer modeling.
The mucin-based proteins the lab develops are “very difficult to see under any microscope or study with experimental techniques within our body, where they are still maintaining physiological conditions,” Chakraborty says. “There are ways, but they’re extremely resource-intensive. So sometimes computation can be a good [way] to model the systems, predict how these proteins will work, and engineer them so that they behave in a way that we want them to.”
This takes a prodigious amount of computing power, and the lab is in the right place for it: Northeastern is home to the Discovery cluster, a network of high-powered servers capable of running thousands of high-volume programs at once, from well-heeled lab research from Chakraborty’s group to undergraduate student projects.
“To do top-of-the-line research you need top-of-the-line equipment,” Chakraborty says. Having that processing power at hand allows the group to run different variations of a given experiment at scale, as well as precise time-lapsed scenarios of how molecules might behave in the body, down to the microsecond.
“It’s much easier to reiterate the studies in computers, rather than having to actually buy the materials, set up labs, and maintain the cleanroom facilities [that biology experiments] require,” says Chakraborty, who joined Northeastern in 2022. Because of that lack of material needs, experiments can be run “infinitely,” she says. “You cannot make that call in a wet lab setting.”
Like building with LEGO blocks
The SymBioSys Lab’s work focuses on glycoproteins — protein molecules with carbohydrates attached that impact any number of functions within the body, including the mucin layer. Mapping out how they work is a critical step in also understanding how many diseases, including cystic fibrosis, operate in the body.
This past fall, the lab received a pair of grants from the National Institutes of Health (NIH) to further that research. The first, a five-year $2 million award through the NIH’s Next Generation Researchers Initiatives, is dedicated to furthering its research on these mucin proteins and developing new biomaterials, with the help of the Discovery cluster. “These materials hold the promise of being customized for various biomedical applications,” the lab’s release on the grant reads. “Like building with molecular LEGO blocks.”
The second (for $100,000) will go toward developing a protein that can deliver gene therapies to treat cystic fibrosis — by getting through the body’s thickened mucin layer. And “we need industry collaborators to test them out,” Chakraborty says. So for the latter project, the lab is working with co-recipient Nanite Bio, a biotech startup founded by former Northeastern chemical engineering professor Shashi Murthy. The company, which has funding from the Cystic Fibrosis Foundation, is dedicated to developing the packaging for these hard-to-administer mRNA treatments. Getting those packages through the body’s mucin layer is where Chakroborty’s lab comes in.



“With cystic fibrosis it’s a huge area of need, because we’ve come a long way in the last 15 or so years, but there are still numbers of patients who can’t be treated with existing drugs,” Murthy says. “We have technologies designed to deliver next generation treatments, like mRNA, but in certain areas of the body it’s very challenging; there’s kind of this last mile problem. We’re able to get to the neighborhood, but [Srirupa] is the one we’re hoping will get us to the mailbox.’’
Murthy says among top-tier research institutions, Northeastern is “unusually friendly” to this sort of academia-industry collaboration. “I started way back in 2005, and over the years I had collaborations with a number of small companies,” he says. Murthy started and sold two startups while on faculty at Northeastern; he now sits on the chemical engineering department’s Industrial Advisory Board, where he first encountered Chakraborty’s research.
Many universities pursue collaboration with corporate giants in various forms, he says, “but the thing that made Northeastern different was its ability to work with startups of different kinds. And that’s a nice sweet spot.”
With cystic fibrosis we’ve come a long way, but there are still numbers of patients who can’t be treated with existing drugs…We’re able to get to the neighborhood, but [Srirupa] is the one we’re hoping will get us to the mailbox.
Shashi Murthy, former Northeastern professor/founder and CEO of Nanite Bio
Effective gene therapy
If it works, the research has the potential to fundamentally upend treatment for cystic fibrosis, which, at present, is limited primarily to management of symptoms.
“The only way right now is improvement in lifestyle, or a cocktail of drugs that help with specific symptoms,” Chakraborty says. “It’s a symptomatic approach of treatment rather than targeting the root cause. However, effective gene therapy could, in theory, be administered to a patient a handful of times and cure the disease.”
Gene therapy itself has already shown promise in other disease areas; biotech giant Novartis has made huge progress on developing gene therapy treatments for leukemia, for example. And in early December, the Food and Drug Administration approved two new gene therapies for sickle cell disease. But with many others, the problem of administering them safely is more complicated than popping a pill or getting a shot, Murthy says. Computer modeling can help game out all manner of different reactions from parts of the body with complex defense systems — the lungs, but also intestinal mucus layers, the blood brain barrier, even certain pockets of the eye.
“You have to be able to solve this last mile problem,” he says. “Otherwise, you have to administer these medicines at doses that are toxic — it’s just not going to work.”
Schuyler Velasco is a Northeastern Global News Magazine senior writer. Email her at s.velasco@northeastern.edu. Follow her on X/Twitter @Schuyler_V.